Table of Contents
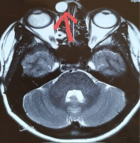
Unusual presentation of oxalate nephropathy causing acute kidney injury: A case report
Published on: 4th November, 2020
OCLC Number/Unique Identifier: 8769674497
Oxalate nephropathy due to Hyperoxaluria and elevated serum oxalate level is a well-known cause for interstitial fibrosis, and ESRD. Conditions associated with high serum Oxalate, should be considered as a possible contributing factor for a patient’s tubular injury.
Well known cause for Hyperoxaluria including enteric Hyperoxaluria (due to gastric bypass, chronic pancreatitis, small Bowel resection, or malabsorption, as well as depletion of enteric oxalate-degrading bacteria [e.g., Oxalobacter). Other known causes of oxalate nephropathy include primary Hyperoxaluria, ethylene glycol intoxication, vitamin B6 deficiency, excessive ingestion of vitamin C or dietary substances rich in oxalic acid, aspergillosis, prolonged renal failure and various drugs (e.g., Known medications to cause Oxalate Nephropathy are: Orlistat, Praxilene, COX-2 inhibitors).
Unusual presentation with Acute Kidney Injury with incidental finding of high serum Oxalate in a patient with a known CKD stage III, recently started on Polyethelene Glycol to treat his constipation.
Modification of the Renal Angina Index for identifying the need for renal replacement therapy in critically ill pediatric patients
Published on: 2nd November, 2020
OCLC Number/Unique Identifier: 8769657642
Severe Acute Kidney Injury (AKI) is a common, serious problem affecting critically ill children that lacks effective treatment options. Currently, there are no treatment options for AKI other than supportive care. Continuous renal replacement therapy (CRRT) is employed to reduce Fluid Overload (FO) burden and treat metabolic disturbances in AKI. Identifying patients upon admission who may require CRRT has potential clinical care implications. The aim of this study was to determine if the RAI had diagnostic capabilities to identify patients who would require CRRT.
The analytic cohort consisted of patients who required CRRT and illness severity score matched controls who did not require CRRT at a single center. Patients who required CRRT had higher mortality rates, length of stay, and use of ventilatory and inotropic support. Sensitivity, specificity and area under the receiver operating characteristic curve (AUC) assessed and compared the discriminatory accuracy of three scores: 1) the renal angina index (RAI), 2) serum-creatinine (sCr) based AKI on day 0 and 3) modified RAI created with an additional RAI injury tranche that corresponded to severe stage 3 AKI sCr elevation.
Compared to Day0AKI (AUC 0.78, 0.70-0.87; sensitivity 0.63, 0.45-0.79; specificity 0.93, 0.870.97) and RAI (AUC 0.76, 0.69-0.82; sensitivity 0.94, 0.81-0.99; specificity 0.57, 0.47-0.66), the modified RAI had the highest AUC (0.79; 0.72-0.85) with a high sensitivity (0.91; 0.77-0.98) and moderate specificity (0.65; 0.56-0.75) for prediction of CRRT requirements. As a more accurate tool for discriminating patients in need of CRRT, a modified RAI has numerous potential implications. Identifying patients who ultimately require CRRT at an earlier timepoint may influence timing of CRRT initiation in an attempt to avoid further FO, or may influence nephrotoxin administration. The diagnostic capabilities of the modified RAI may be refined by the addition of urinary biomarkers. These findings should be validated in a larger cohort.
COVID-19 related rhabdomyolysis
Published on: 20th October, 2020
OCLC Number/Unique Identifier: 8691888726
A novel coronavirus known as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) with a high rate of human-to-human transmission has emerged, resulting in a worldwide public health crisis of catastrophic proportions. Common initial symptoms of Coronavirus Disease 2019 (COVID-19) include fever, cough, fatigue, myalgia, and shortness of breath. Complications include acute respiratory distress syndrome (ARDS), acute cardiac injury, acute kidney injury, and secondary infections [1,2]. There have been reports of patients infected with COVID-19 who either presented with muscle pain and rhabdomyolysis or developed muscle damage as a late complication during hospitalization [3-8].
Frequency of renal tubular acidosis in children with down syndrome
Published on: 2nd October, 2020
OCLC Number/Unique Identifier: 8691889815
Background: Down syndrome (DS) is associated with various congenital diseases and malformations, including those of the kidneys and urinary tract. It has been thought that renal tubular acidosis (RTA) is more frequent in this population. The objective of this study was to assess the frequency of RTA and, secondarily, of other renal and urological disorders in persons with DS.
Method: An observational, ambispective, descriptive and cross-sectional study of patients diagnosed with RTA, or suspected kidney or urological disorders, was carried out from July 2016 to September 2017 at the Down syndrome clinic of the Mexican National Institute of Paediatrics. Urinalysis was performed, along with analyses of venous blood gas, sodium, potassium, chlorine, calcium, phosphorus, albumin and creatinine. Those with any abnormal values were referred to nephrology for diagnostic evaluation.
Results: Of a total of 700 patients seen at the clinic, 47 met the selection criteria. Of these, 32 had no RTA or other renal or urological alterations. The remaining 15 continued to the second phase of the study, where 6 were diagnosed with nephropathy or uropathy (RTA, systemic arterial hypertension, monosymptomatic familial haematuria, mild renal failure secondary to reflux nephropathy, urinary tract infection or right ureteropelvic stenosis). Four had mild metabolic acidosis without meeting the criteria for diagnosis of RTA.
Conclusion: RTA is not more common in children with Down syndrome. Nephropathies and uropathies should be investigated in the evaluation of DS patients.
Acute kidney injury in Colombian patients with COVID-19 who received kidney support therapy with genius® 90 technology
Published on: 11th September, 2020
OCLC Number/Unique Identifier: 8665847570
Introduction: Acute kidney injury (AKI) is one of the complications associated with severe COVID-19 infection, and it can present in up to 20% to 40% of the cases; of these, approximately 20% will require renal replacement therapy (RRT).
Objective: To establish clinical and laboratory characteristics in a group of patients from Colombia with COVID-19 infection and AKI that received intermittent and prolonged RRT with the GENIUS® 90 technology in between March and July 2020.
Design: Cross-sectional study.
Results: 78.9% of participants were men and 21.1% were women. The main comorbidities were the following: Hypertension (65.3%), diabetes mellitus (38.9%), obesity (26.3%), cancer (5.3%), Chronic obstructive pulmonary disease (11.6%), cardiovascular disease (23.2%), active smoking (11.6%). 33.7% had chronic kidney disease (CKD) in the average serum creatinine on admission was 4.4 mg/dl.
The following inflammatory markers were elevated: C-reactive protein (CRP), d-dimer and ferritin (20.3 mg/dl, 931mcg/l and 1174 ng/ml, respectively). 63.5% of patients underwent sustained low-efficiency dialysis (SLED) (6 to 12 hours) and the rest of the patients (36.35%) underwent conventional hemodialysis (less than 4 hours). The mortality of the total patient sample was 36.9%, lower in patients with CKD than in patients with no previous renal disease history (18.7% and 40.1%, respectively).
Conclusion: Renal complications are frequent in patients with severe COVID-19. The development of AKI could be an isolated prognostic marker associated with an increase in mortality in patients with COVID-19, and one of the options is intermittent and prolonged RRT with the GENIUS® 90 system.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."