More Information
Submitted: October 27, 2022 | Approved: November 02, 2022 | Published: November 03, 2022
How to cite this article: Ledesma G, Rivas B, Vega C, Carreño G, Trigo E, et al. Strongyloides stercoralis and glomerular diseases: A case report. J Clini Nephrol. 2022; 6: 097-098.
DOI: 10.29328/journal.jcn.1001099
Copyright License: © 2022 Ledesma G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Strongyloides; Strongyloidiasis; Glomerulonephritis; Inmunosuppression
Strongyloides stercoralis and glomerular diseases: A case report
Gabriel Ledesma1*, Begoña Rivas2, Cristina Vega2, Gilda Carreño2, Raquel Díaz1, Ángel Gallegos1, Verónica Mercado1, Silvia Caldés1, Yesika Amezquita1, Yolanda Hernández1, Rocío Echarri1, Covadonga Hevia1 and Antonio Cirugeda1
1Nephrology Department, Infanta Sofia University Hospital, Madrid, Spain; European University of Madrid School of Medicine, Madrid, Spain
2Nephrology Department, La Paz University Hospital, Madrid, Spain
*Address for Correspondence: Gabriel Ledesma, Nephrology Department, Infanta Sofia University Hospital, Madrid, Spain; European University of Madrid School of Medicine, Madrid, Spain, Email: [email protected]
Strongyloidiasis is an intestinal parasitic infection caused by the nematode Strongyloides stercoralis. It is endemic in rural tropical and subtropical areas with a prevalence of 100 million people worldwide [1]. In Spain, we find endemic areas at several points on the Mediterranean coast [2].
It produces a paucisymptomatic infection except in situations of immunosuppression, in which it can lead to massive dissemination of the larva with a risk of death. Hence the importance of suspecting this entity in patients with epidemiological risk factors under immunosuppressive treatment.
We present a case of a 44 – years - old woman from Bolivia, resident in Spain since 2008. Her medical history includes a meningioma treated with radiotherapy and four pregnancies, the last one in 2014, complicated by preeclampsia. Cesarean section was performed and after 8 weeks subnephrotic proteinuria persisted together with microhematuria, with normal renal function and normal immunological profile. A renal biopsy was performed with the result of IgA nephropathy (IgAN), starting prednisone at a dose of 1 mg/kg/day.
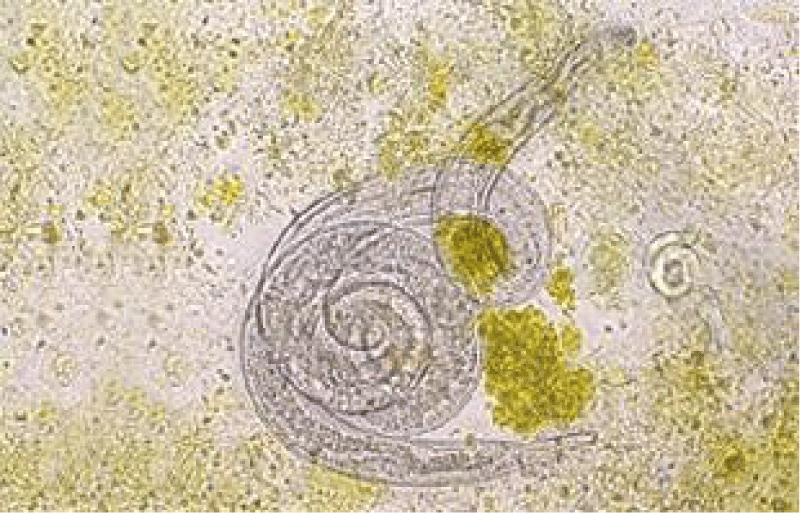
One month after starting prednisone, the patient traveled to Bolivia for two weeks. Upon his return, she presented a fever of unknown origin and generalized itching, for which microbiological tests were requested with a positive result for Strongyloides stercoral in serial stool examination (Figures 1,2). A tapering regimen of glucocorticoids was started and ivermectin (200 mcg/kg/day) was administered orally. She didn’t present eosinophilia at any time. Monitoring of response to treatment was performed by serology (ELISA test). At diagnosis, IgG titer was 2.97 (positive > 0.3) and progressively decreased in a few months (1.77 after one month and 0.63 after 4 months of treatment with ivermectin).
Figure 1: Strongylodes stercoral in stool examination.
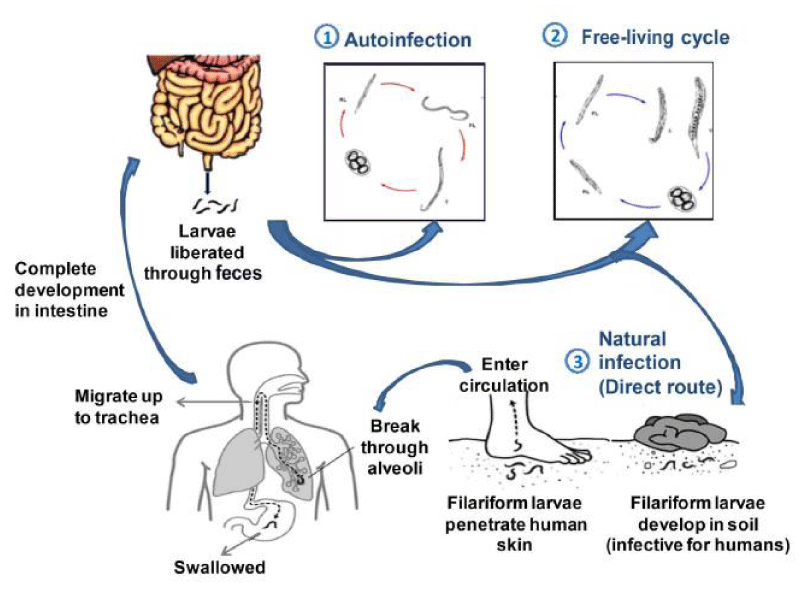
Figure 2: Life cicle of Strongyloides stercolaris [10].
Strongylodes stercoral is a parasite with an atypical life cycle that differentiates it from the rest of the helminths by being able to complete it without abandoning the host, that is, with the capacity for autoinfection.
Autoinfection is limited in immunocompetent patients, which prevents the disease but not the life cycle within the host, which lasts for years without causing symptoms except fluctuating eosinophilia [2]. It is in a situation of immunosuppression (especially induced by corticosteroids) when the cycle goes out of control and the dissemination of the parasite increases throughout the body, giving varied and non-specific manifestations. The most frequently affected organs are the skin, the gastrointestinal tract, and the respiratory system. The most severe form of Strongyloidiasis is hyperinfestation syndrome due to the massive dissemination of the filariform larva, endangering the life of the patient.
Diagnosis is made by direct visualization of the larva in a biological sample (faeces, bronchoalveolar lavage, duodenal biopsy) or by indirect ELISA test. In immunosuppressed patients, eosinophilia may be absent and serology may give false negatives.
The drug of choice is ivermectin, followed by albendazole as second-line treatment, both being able to be combined in hyperinfestation syndrome (in addition to withdrawing immunosuppression) [3]. The response is monitored by stool examination, antibody titer, and degree of eosinophilia. If there is refractoriness to treatment, we must rule out HTVL-1 co-infection.
In the case we present, the rapid diagnostic and therapeutic action managed to prevent a progression of the infection that could have led to hyperinfestation syndrome. Reviewing the literature, the association between this syndrome and delay in diagnosis is reflected, with published cases being frequent in renal transplant recipients, but rare in patients with acute glomerulonephritis. Among them, we found cases of type I membranoproliferative glomerulonephritis [4-6], ANCA-MPO vasculitis [7], or lupus nephropathy [8]. All of them share common characteristics: corticosteroid therapy (in addition to cyclophosphamide), absence or minimal eosinophilia, exposure in endemic areas (sometimes decades ago), nonspecific symptoms (especially fever, respiratory symptoms or digestive symptoms) and diagnosis with invasive methods (biopsy intestinal, bronchoalveolar lavage) due to low initial suspicion of parasitosis. Exceptionally, we found a described case of Strongyloidiasis in an asymptomatic patient with IgAN who received ivermectin before treatment with corticosteroids [9].
We must remember that many glomerulonephrites occur within systemic diseases, with nonspecific symptoms common to Strongyloidiasis, which can lead to an erroneous increase in immunosuppression. Mora, et al. [8] insist on this aspect, she published a series of cases of hyperinfestation syndrome in patients with systemic lupus erythematosus in whom immunosuppression was initially increased due to suspected lupus activity, with clinical worsening and, in some cases, death.
In patients from endemic areas for Strongyloides stercoralis who are going to receive immunosuppression, prior screening of Strongyloidiasis and other parasitic infections should be performed and, in confirmed cases, treated, so they may complicate the patient’s prognosis. Immunocompromised patients with fever of unknown origin who have not been screened before treatment and who come from an endemic area should also be studied, even if they have not presented diarrhea or eosinophilia.
- World Health Organization. 2018. http://www.who.int/intestinal_worms/epidemiology/Strongyloidiasis/en/
- Pacheco-Tenza MI, Ruiz-Maciá JA, Navarro-Cots M, Gregori-Colomé J, Cepeda-Rodrigo JM, Llenas-García J. Strongyloides stercoralis en un hospital comarcal del Levante español: una enfermedad no solo importada. Enferm Infecc Microbiol Clin. 2017.
- Segarra-Newnham M. Manifestations, diagnosis, and treatment of Strongyloides stercoralis infection. Ann Pharmacother. 2007 Dec;41(12):1992-2001. doi: 10.1345/aph.1K302. Epub 2007 Oct 16. PMID: 17940124.
- Malakoutian T, Mohammadi R, Asgari M, Amouzegar A. Disseminated Strongyloidiasis in a patient with membranoproliferative glomerulonephritis-case report. Iran J Parasitol. 2015 Jan-Mar;10(1):141-5. PMID: 25904959; PMCID: PMC4403535.
- Gluhovschi G, Gluhovschi C, Velciov S, Ratiu I, Bozdog G, Taban S, Petrica L. "Surprise" in the evolution of chronic membranoproliferative glomerulonephritis associated with severe Strongyloidiasis under corticotherapy: "hygienic paradox"? Ren Fail. 2013 Aug;35(7):1017-23. doi: 10.3109/0886022X.2013.810103. Epub 2013 Jul 5. PMID: 23826871.
- Sathe PA, Madiwale CV. Strongyloidiasis hyperinfection in a patient with membranoproliferative glomerulonephritis. J Postgrad Med. 2006 Jul-Sep;52(3):221-2. PMID: 16855328.
- Rajapurkar M, Hegde U, Rokhade M, Gang S, Gohel K. Respiratory hyperinfection with Strongyloides stercoralis in a patient with renal failure. Nat Clin Pract Nephrol. 2007 Oct;3(10):573-7. doi: 10.1038/ncpneph0598. PMID: 17895934.
- Mora CS, Segami MI, Hidalgo JA. Strongyloides stercoralis hyperinfection in systemic lupus erythematosus and the antiphospholipid syndrome. Semin Arthritis Rheum. 2006 Dec;36(3):135-43. doi: 10.1016/j.semarthrit.2006.06.001. Epub 2006 Sep 1. PMID: 16949135.
- Gravellone L, Battaglia C, Caligara F, D'Amato I, Gandini E, Lucatello A, Rizzo MA, Torpia R, Brigante G, Castiglioni A. Strongiloidosi: la cenerentola delle parassitosi. due casi emblematici in pazienti nefrologici [Strongyloidiasis in nephrologic patients]. G Ital Nefrol. 2015 Mar-Apr;32(2):gin/32.2.26. Italian. PMID: 26005937.
- Puthiyakunnon S, Boddu S, Li Y, Zhou X, Wang C, Li J, Chen X. Strongyloidiasis--an insight into its global prevalence and management. PLoS Negl Trop Dis. 2014 Aug 14;8(8):e3018. doi: 10.1371/journal.pntd.0003018. PMID: 25121962; PMCID: PMC4133206.