More Information
Submitted: September 30, 2022 | Approved: October 04, 2022 | Published: October 05, 2022
How to cite this article: Montepío RP, Gonzales BM, Villa JDJ. Accidental placement of hemodialysis catheter tip in the right internal mammary vein: a case report. J Clini Nephrol. 2022; 6: 094-096.
DOI: 10.29328/journal.jcn.1001098
Copyright License: © 2022 Montepío RP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Accidental placement of hemodialysis catheter tip in the right internal mammary vein: a case report
Rafael Parcarey Montepío1,2*, Bernardo Moguel Gonzales1 and Jose Daniel Juarez Villa1
1Nephrology Department, National Institute of Cardiology, Mexico City, Mexico
2Nephrology Department, National Kidney and Transplant Institute, Philippines
*Address for Correspondence: Rafael Parcarey Montepio, MD, Interventional Nephrology Fellow (ISN scholar), National Institute of Cardiology “Ignacio Chavez”, Mexico City, Mexico, Email: [email protected]; [email protected]
Hemodialysis catheter placement, particularly Internal Jugular Catheter insertion, is a very common procedure for patients who require urgent access to renal replacement therapy. Most of these procedures are done under ultrasound guidance as recommended by KDIGO 2019 vascular access guidelines. However, catheter tip misplacement can still occur even in the experts’ hands and despite the use of ultrasound. In this case report, we will discuss a hemodialysis catheter tip placement in the right internal mammary vein and how we managed it.
Central venous placement is an important procedure not just for access to hemodialysis patients but also for critically-ill patients, for infusion of intravenous fluids, medications, and central venous pressure monitoring. Over 80% of new hemodialysis patients are initiated with hemodialysis catheters, despite guidelines recommending early planning for arteriovenous access to minimize catheter use [1-3]. Ultrasound guidance is highly recommended in performing these procedures, but it is not without risks. Published rates of cannulation success and complications vary according to the anatomic site, the use of ultrasound guidance and operator experience. One review described an overall complication rate of 15% [4]. The following are the common immediate complications: pneumothorax, venous air embolism, arterial injury and arrhythmia. Accidental insertion of an internal mammary vein is a very rare complication, estimated to occur in only 1% to 2% of cases [5,6]. Most of these case reports are accidental misplacement into the left internal mammary vein through a left internal jugular catheter insertion [6-9]. Case reports of inadvertent insertions into a right internal mammary vein are secondary to cannulations of either the left internal jugular vein or subclavian vein [10,11]. Inadvertent insertion of a right internal mammary vein from a right internal jugular vein cannulation is even less likely to happen because the right internal jugular vein has a more straight path going to the superior vena cava, making our case report more rare and unique.
A 57-year-old male, diagnosed with Chronic Kidney Disease stage 5 secondary to Diabetic Kidney Disease, on hemodialysis for 4 years (2018), three times a week (Monday, Wednesday, and Friday), with multiple histories of hemodialysis catheter placement (1st and 2nd: right internal jugular, non-tunneled-removed due to malfunction, both lasted less than a month; 3rd: left internal jugular vein, non-tunneled-removed due to infection, lasted approximately for 8 months; 4th: right femoral vein, non-tunneled, lasted for less than a month and the 5th: left tunneled internal jugular catheter, inserted 3 years ago). The patient underwent removal of the left tunneled internal jugular catheter with subsequent insertion of a temporary (non-tunneled) catheter on the right side. The indication of removal was a catheter malfunction for the past 2 weeks-only a maximum blood flow rate (Qb) of 150 ml/min can be delivered during hemodialysis. No fibrinolytic therapy was given. Catheter blood-stream infection was not considered due to the absence of symptoms. Chest X-ray showed the placement of the tip in the superior vena cava. He was eventually referred to our institution for further evaluation and management. The procedure was done as an outpatient. A new temporary internal jugular catheter had to be inserted because the patient was scheduled for dialysis the next day. The reason why Arterio-Venous Fistula (AVF) was not yet done is unknown to us and the patient. The patient came from another government hospital in Mexico and was new to our institution.
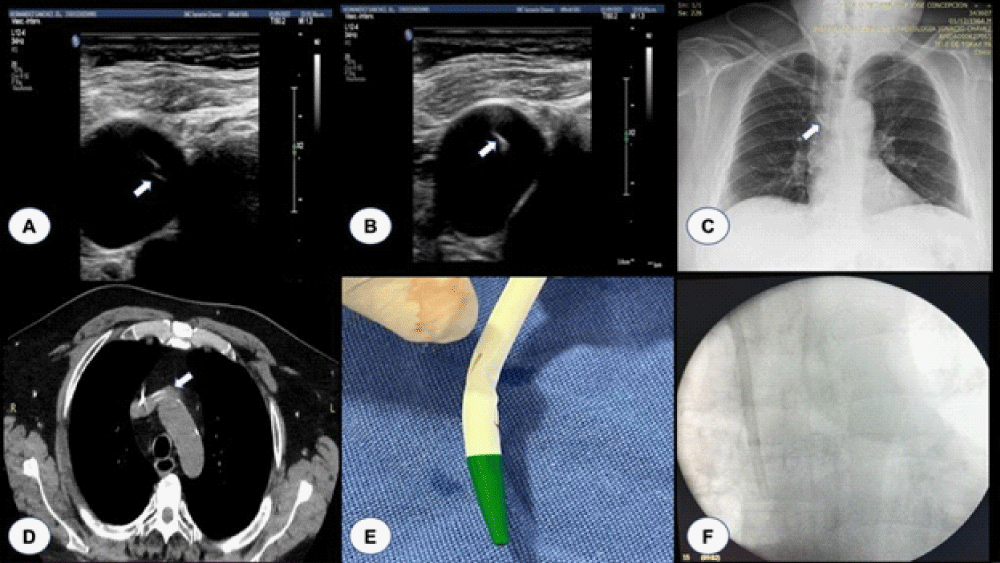
Pre-operative ultrasound of both jugular veins showed the presence of thrombosis, more on the left. Hence, the temporary catheter was inserted into the right Internal Jugular vein. Right-sided Internal Jugular catheter cannulation was successfully achieved with ultrasound guidance (Figures 1A and 1B). Resistance was noted when the guidewire was inserted beyond 15 cm. The plan was to insert the guidewire up to 20 cm and the catheter at 16 cm levels. Inserting the catheter beyond 15 cm was associated with the symptom of chest pain. Hence, the catheter was inserted and sutured only at this level. He was asymptomatic at this level, and aspiration of blood and flushing with saline could be done without resistance. Possible stenosis or obstruction was suspected because of the resistance noted. A chest X-ray seems unremarkable, with a tip at the superior vena cava (Figure 1C). But because of a high index of suspicion, a Chest CT scan with contrast was also requested which revealed that the distal end of the hemodialysis venous catheter tip was located in the internal mammary vein, and no data suggestive of superior vena cava stenosis (Figure 1D). The patient had his hemodialysis the next day and it was noted that he could only tolerate a blood flow rate of 150 ml/min. Manipulation was done by the nephrology fellow and nurse on duty, pulling out 2 cm to 3 cm of the catheter, which eventually increased the blood flow rate to 250 ml/min. The patient was asymptomatic during hemodialysis. The following week, the patient was scheduled for a tunneled catheter insertion under fluoroscopy to make sure that the tip would be inserted correctly. Intraoperative findings showed a distorted internal jugular catheter tip (Figure 1E), with the catheter already pulled out at around 13 cm. The procedure was done successfully with a tip noted at the superior vena cava (Figure 1F).
Figure 1: A: Needle in the middle of the vein; B: Guidewire; C: Chest X-ray post IJ catheter insertion; D: Chest CT scan with contrast; E: IJ catheter removed during fluoroscopy; F: Final catheter insertion after the fluoroscopy.
Accidental insertion of the hemodialysis catheter tip into an internal mammary vein is a very rare complication, estimated only to occur in 1% - 2% of cases [5,6]. On our literature search, almost all of the case reports noted malposition in the left internal mammary vein [6-9]. Case reports of inadvertent insertions into a right internal mammary vein are secondary to cannulations of either the left internal jugular vein or subclavian vein [10,11]. Inadvertent insertion of a right internal mammary vein from a right internal jugular vein cannulation is even less likely to happen because the right internal jugular vein has a more straight path going to the superior vena cava, making our case report more rare and unique.
The internal mammary vein receives the anterior intercostal veins as well as some abdominal branches, eventually draining into the brachiocephalic vein behind the sternal end of the clavicle and the first costal cartilage [5,6]. One of the possible causes of malposition of the internal mammary vein is the presence of portal hypertension, due to the dilatation of the collateral veins from the portal system. However, we were not entertaining the presence of portal hypertension in our patient. A possible explanation could be the dilatation of collateral veins secondary to the previous history of repeated central venous catheterization. Nonetheless, a definite etiology remains unclear.
Our patient complained of chest pain upon guidewire insertion beyond 15 cm. This was also accompanied by resistance on that same level. These could be the early sign and symptoms of catheter malposition into the internal mammary vein. The ultrasound-guided us in inserting the catheter into the Internal Jugular vein, but it does not guarantee that the tip would be correctly inserted in the aortocaval area. The Chest X-ray was also not helpful in ruling out internal mammary vein insertion, as shown in our case. Hence, for suspicion of catheter tip malposition, a chest CT scan with contrast, CT angiography, or fluoroscopy should be done to confirm the tip placement.
Ultrasound has significantly improved the success of Internal Jugular catheterization. One prospective randomized controlled trial, significantly decreased failed cannulation rate from 35% to 0% [12]. Another prospective randomized controlled trial noted an improvement in successful cannulation rate from 76% to 100% with the use of real-time ultrasound guidance [13]. However, our case report only proves that even if we successfully cannulated the internal jugular vein, catheter tip malposition is still a possible complication, that requires a high index of suspicion.
Urgent interventions should be done once central venous catheter tip malposition to the internal mammary vein is confirmed, because of the risk of perforation of that vessel and extravasation of blood and fluids into the surrounding tissue. An increased risk of thrombosis is also likely because of a low flow state. While there are still no clear guidelines on how to manage this case, we think that the best approach should be to reinsert the catheter through the guidance of fluoroscopy, as we did to our patient.
Accidental cannulation of the internal mammary vein is a very rare complication of Internal Jugular catheter insertion. An inadvertent right internal mammary vein malposition from a right internal jugular vein cannulation is probably even rarer since the right Internal Jugular catheter should go straight down to the superior vena cava. This case report showed that this complication is possible even with the use of ultrasound guidance. Once there is a high index of suspicion, the insertion of the tip should be confirmed by a CT scan or fluoroscopy, and the catheter should be removed as soon as possible. Further studies should be done to establish a more definitive guideline.
- Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, Allon M, Asif A, Astor BC, Glickman MH, Graham J, Moist LM, Rajan DK, Roberts C, Vachharajani TJ, Valentini RP; National Kidney Foundation. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020 Apr;75(4 Suppl 2):S1-S164. doi: 10.1053/j.ajkd.2019.12.001. Epub 2020 Mar 12. Erratum in: Am J Kidney Dis. 2021 Apr;77(4):551. PMID: 32778223.
- O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S; Healthcare Infection Control Practices Advisory Committee (HICPAC) (Appendix 1). Summary of recommendations: Guidelines for the Prevention of Intravascular Catheter-related Infections. Clin Infect Dis. 2011 May;52(9):1087-99. doi: 10.1093/cid/cir138. PMID: 21467014; PMCID: PMC3106267.
- Smith RN, Nolan JP. Central venous catheters. BMJ. 2013 Nov 11;347:f6570. doi: 10.1136/bmj.f6570. PMID: 24217269.
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003 Mar 20;348(12):1123-33. doi: 10.1056/NEJMra011883. PMID: 12646670.
- Wang L, Liu ZS, Wang CA. Malposition of Central Venous Catheter: Presentation and Management. Chin Med J (Engl). 2016 Jan 20;129(2):227-34. doi: 10.4103/0366-6999.173525. PMID: 26830995; PMCID: PMC4799551.
- Munta K, Venkategowda PM, Chaudhary JR, Rao SM, Amte R. Accidental placement of central venous catheter tip into internal mammary vein. Indian J Crit Care Med. 2015 Jun;19(6):365-6. doi: 10.4103/0972-5229.158290. PMID: 26195868; PMCID: PMC4478683.
- Goodin P, Jain N, Jeelani HM, Bharat A. Accidental Central Venous Catheter Placement in the Internal Thoracic Vein: A Case Report. Cureus. 2020 Jul 18;12(7):e9255. doi: 10.7759/cureus.9255. PMID: 32821601; PMCID: PMC7430698.
- House LM 2nd, Yen A, Bokoch MP. Central Venous Catheter in the Internal Mammary Vein. Anesthesiology. 2019 Aug;131(2):397. doi: 10.1097/ALN.0000000000002702. PMID: 30973515.
- Mon W. Misplacement of Central Venous Catheter into the Left Internal Mammary Vein. Anaesthesia Cases. 2016; 0224:102-105.
- Sakan S, Basić-Jukić N, Kes P, Stern-Padovan R, Perić M. Malposition of central venous dialysis catheter in the right internal mammary vein in uremic patient: case report. Acta Clin Croat. 2011 Dec;50(4):623-6. PMID: 22649898.
- Tristão FR, Moreira RCR, Valle CED, Neves GCS. Inadvertent insertion of a venous catheter into the internal thoracic vein: a word of caution. J Vasc Bras. 2019 Nov 18;18:e20190097. doi: 10.1590/1677-5449.190097. PMID: 31807130; PMCID: PMC6880616.
- Mallory DL, McGee WT, Shawker TH, Brenner M, Bailey KR, Evans RG, Parker MM, Farmer JC, Parillo JE. Ultrasound guidance improves the success rate of internal jugular vein cannulation. A prospective, randomized trial. Chest. 1990 Jul;98(1):157-60. doi: 10.1378/chest.98.1.157. PMID: 2193776.
- Slama M, Novara A, Safavian A, Ossart M, Safar M, Fagon JY. Improvement of internal jugular vein cannulation using an ultrasound-guided technique. Intensive Care Med. 1997 Aug;23(8):916-9. doi: 10.1007/s001340050432. PMID: 9310813.