More Information
Submitted: May 26, 2021 | Approved: July 13, 2021 | Published: July 14, 2021
How to cite this article: Diab A, Anthony P, Berryman H, Diab K. Acute Kidney Injury due to spontaneous Atheroembolic disease, superimposed on diabetic nephropathy, with no recent vascular or cardiac intervention, presented as Rapidly Progressive Glomerulonephritis (RPGN). J Clini Nephrol. 2021; 5: 053-055.
DOI: 10.29328/journal.jcn.1001074
Copyright License: © 2021 Diab A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Acute Kidney Injury due to spontaneous Atheroembolic disease, superimposed on diabetic nephropathy, with no recent vascular or cardiac intervention, presented as Rapidly Progressive Glomerulonephritis (RPGN)
Anas Diab*, Parravani Anthony, Hollie Berryman and Kareem Diab
Department of Medicine, Section of Nephrology, Morgantown, WV 26506, USA
*Address for Correspondence: Anas Diab, Department of Medicine, Section of Nephrology, 4th Floor, HSCN Room 4076A, Morgantown, WV 26506, USA, Tel: 304-293-2551; Fax: 304-293-7373; Email: [email protected]
Atheroembolic disease (AED), or Cholesterol Crystals Embolism, is a systemic disease presented as a complication of severe atherosclerosis [1], where older age, male sex, diabetes hypercholesterolemia, smoking and hypertension [2], are the main risk factors for the development of Atherosclerosis, it is known that spontaneous atherosclerotic renal disease is rare in the absence of any vascular intervention [3], and in the absence of anticoagulant [4], or the absence of calcified aorta, with the most common presentation of the disease is subacute kidney injury progress into renal dysfunction occurs in like a staircase pattern and the renal dysfunction is usually observed several weeks after a possible intervention, caused by dislodging the micro cholesterol plaques from a major artery, and start showering multiple organs causing micro and macro embolic phenomena.
In our case, we report acute kidney injury on a previously stable kidney disease in a female with diabetes mellitus type 2 presented with severe anemia, dyspnea, massive fluid overload with bilateral pleural effusion, patient had a history of multiple IV contrast exposures, with peripheral vascular occlusive disease (PVOD), required amputation of right below the knee amputation, presented during the COVID-19 pandemic, found with nephrotic syndrome, a kidney biopsy has shown cholesterol crystal embolization compatible with Athero-embolic Disease with severe Diabetic Nephropathy.
57 years old, female, ex-smoker, admitted for progressive exertional dyspnea over several weeks in addition to orthopnea and lower extremity edema.
At outside facility, she was found to be anemic with Hgb 6 gm/dl. Transferred to West Virginia/Ruby Memorial Hospital, with suspected etiology of her respiratory compromise to be acute exacerbation of underlying CHF, treated for massive fluid overload with Intravenous Albumin, Furosemide and Oral Metolazone, with good response on her Urine Output averaged 3-4 Liters /day, with improvement in her Respiratory status resolving of her Peripheral Edema within 5-6 days from the time of admition.
Serum creatinine 4.1 mg/dL upon presentation with her baseline serum Creatinine appeared to be 1.1-0.9 mg/dl, 6 months prior to admition, and discharged Serum Creatinine with no improvement at 4.1 mg/dl with estimated Glomerular Filtration Rate (GFR) 11 ml/min, patient did not require Renal Replacement Therapy. No anticoagulant was used during the admition given to prevent DVT given that her presentation with severe anemia and the possibility of Gastro-intestinal bleeding, her Aspirin was stopped as well.
Past medical history with poorly controlled diabetes and uncontrolled hypertension for many years, history of chronic Non-Steroidal Anti-Inflammatory Drugs (NSAID) use, and multiple exposures to IV contrast and antibiotics. Other medical problems include Peripheral Vascular Occlusive Disease (PVOD), post right above the Knee Amputation (AKA), hyperlipidemia, diastolic heart failure, and hypothyroidism after Radio-Iodine treatment for Thyrotoxicosis.
Her physical exam: showed BP 156/87, RR 24/min, few bibasilar rales, no abdominal vascular bruit, left lower extremity with 2+ pitting edema, right above the knee amputation, left foot with no livedo reticularis, diminished pulse in the dorsalis pedis.
Serum sodium 134 millimole per L, Potassium 3.9 millimole per L, Carbon Dioxide 18 millimole per L Blood Urea Nitrogen (BUN) 69 mg/dL Glucose 187 mg per dL Calcium 8 mg/dL Phosphorus 7.4 mg/dL C-reactive Protein 72 milligram/liter. Serum Albumin 1.4 gm/dl, with total Cholesterol 252 mg/dl, Low Density Lipoprotein (LDL) 127 mg/dl, and Triglyceride 507 mg/dl.
Urinalysis with Glucose more than 500, small amount of Blood, massive Protein.
Random Urine Protein to Creatinine ratio (UPC) 18.
She had a negative test for HIV.
Repeat Trans Thoracic Echocardiogram (TTE), revealed newly reduced Left Ventricular Ejection Fraction (LVEF) at 48% with multiple akinetic segments and a moderate pericardial effusion. Renal Ultrasound with normal finding, Urine and Serum Protein Electrophoresis (UPEP/SPEP) with no M spike on Electrophoresis, Myeloperoxidase Antibodies (MPO) Anti-Neutrophilic Cytoplasmic Antibodies (ANCA) IgG were negative, Perinuclear Antineutrophil Cytoplasmic Antibody (PR3) was unremarkable.
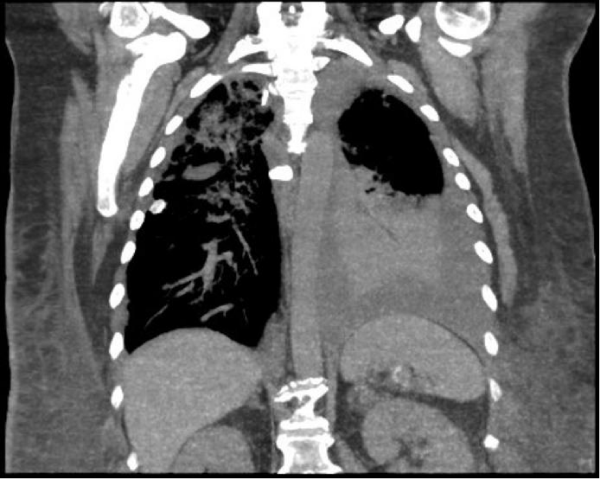
CT scan of her Thorax did not show any descending aortic calcification, significant Left Pleural Effusion, Pleural and pericardial effusions analysis were deemed transudative (Figure 1).
Figure 1: CT scan.
CT abdomen, with few calcifications at the origin of the renal arteries (Figure 2).
Figure 2: CT scan.
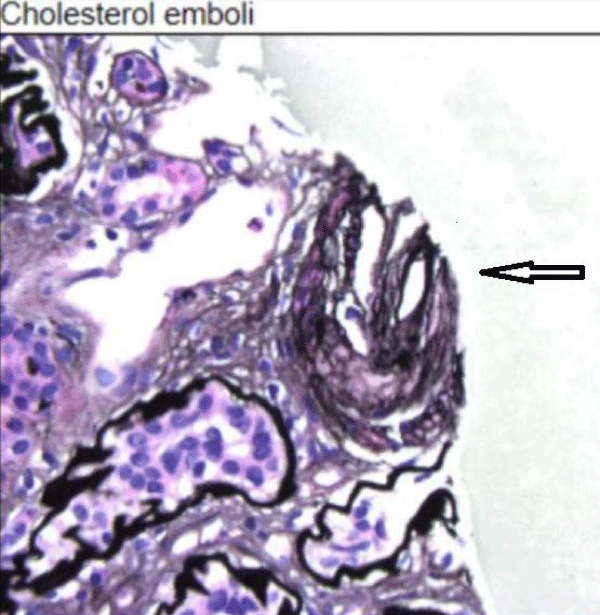
A Kidney Biopsy was performed from her Left Kidney, and revealed advanced Diabetic with glomeruli show well-formed Kimmelstiel Wilson nodules with nodular mesangial expansion and no significant increase in mesangial cellularity Glomerulosclerosis, with features suggesting Aeroembolism events, segmental sclerosis, arteriosclerosis with severe interstitial fibrosis and tubular atrophic changes in approximately 70% - 80% of the cortex Several arteries and arterioles show needle shaped cholesterol clefts. No vasculitis is present (Figure 3).
Figure 3: Kidney Biopsy.
Examination of a glomerulus by electron microscopy shows patent capillary loops, the glomerular capillary basement membranes are thickened up to 3-5 times normal. Mesangial matrix expansion is noted. There is severe foot process effacement of the podocytes. No immune type electron dense deposits are seen along the glomerular capillary loops or in the mesangial areas. The tubular basement membranes are markedly thickened but without deposits.
This is unusual presentation, for Acute Kidney Injury, with Nephrotic Syndrome, and Hematuria in a middle age ex-smoker female, with Uncontrolled Diabetes, and Hypercholesterolemia presented with severe exertional dyspnea in the absence of cardiac events, found with Nephrotic syndrome (mostly from her Diabetic Nephropathy), and hematuria, and given the rapid decline in her kidney functions during the period proceeding her hospitalization with negative vasculitis or Acute Interstitial Nephritis work up, apparent volume overload, responded well to Diuresis, a kidney biopsy was performed and showed severe Aeroembolism disease.
The absence of any other indicators like calcification of the aorta [5], and absence of peripheral sign like Livedo reticularis, work up for Atheroembolic Disease was not performed initially: LDH, C3, C4 [6], CRP [7] given that it was not expected, the disease was limited only to the kidneys, patient was discharged after she was treated for fluid overload, with advanced Chronic Kidney Disease, and to plan for future renal replacement therapy.
An explanation for the presence of Hematuria, with no urinary RBC’s casts, can be explained by the nature of AED, where it is caused by occlusion of small arteries in the kidney by Cholesterol Crystal Emboli from ulcerated Atherosclerotic Plaques, which can mimic microinfarction of the kidneys, and causing hematuria [8]. A question for future investigator should address if hematuria is a specific marker to assess the extent of this disease.
A kidney biopsy is not regularly considered as a routine procedure in someone with a long-standing history of uncontrolled Diabetes Mellitus, but in this case the rapid decline in kidney functions, and the presence of Nephrotic syndrome with Hematuria, presented as a Nephritic/Nephrotic syndrome, justify doing the kidney biopsy, which has been essential in making diagnosis, and it should be considered in future cases with unexplainable rapid decline in kidney functions. Still there is no definitive answer to perform a kidney biopsy if the same presentation but with normal kidney functions, the yield of the kidney biopsy may have overall more risk than benefit.
Glomerular Endothelial injury represents a critical pathological process in the development of Glomerular sclerosis, and unfortunately in this case it was not evaluated, by the electron microscopy.
Work up in the future should include Cystoscopy to look at lower urinary causes, especially in a previous heavy smoker patient, since there is no association between AED and Hematuria.
In conclusion AED Nephritis, should be suspected in Uncontrolled Diabetes Mellitus, smoker, and severe hyperlipidemia, even in the absence of recent vascular intervention, and absence of physical signs: Livedo Reticularis [9], and a routine CRP, LDH and Serum Complement levels need to be checked in all patients presented with AKI associated with Hematuria, and having the previously mentioned risk factors.
- Kronzon I, Saric M. Cholesterol embolization syndrome. Circulation 2010; 122: 631-641. PubMed: https://pubmed.ncbi.nlm.nih.gov/20697039/
- Tanaka H, Yamana H, Matsui H, Fushimi K, Yasunaga H, et al. Proportion and risk factors of cholesterol crystal embolization after cardiovascular procedures: a retrospective national database study. Heart Vessels 2020; 35:1250-1255. PubMed: https://pubmed.ncbi.nlm.nih.gov/32277287/
- Nickol J, Richards T, Mullins J. Cholesterol Embolization Syndrome From Penetrating Aortic Ulcer. Cureus 2020; 12: e8670. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7370687/
- Muller-Hansma AHG, Daemen-Gubbels CRGM, Schut NH. Cholesterol embolisms as possible adverse drug reaction of direct oral anticoagulants. Neth J Med 2018; 76:125-128. PubMed: https://pubmed.ncbi.nlm.nih.gov/29667588/
- Scolari F, Ravani P. Atheroembolic renal disease. Lancet 2010; 375: 1650-1660. PubMed: https://pubmed.ncbi.nlm.nih.gov/20381857/
- Cosio FG, Zager RA, Sharma HM. Atheroembolic renal disease causes hypocomplementaemia. Lancet 1985; 2: 118-121. PubMed: https://pubmed.ncbi.nlm.nih.gov/2862317/
- Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, et al. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005; 352: 20-28. PubMed: https://pubmed.ncbi.nlm.nih.gov/15635109/
- Vaidya PN, Finnigan NA. Atheroembolic Kidney Disease. 2021. PubMed: https://pubmed.ncbi.nlm.nih.gov/29494024/
- Matsumura T, Matsumoto A, Ohno M, Suzuki S, Ohta M, et al. A case of cholesterol embolism confirmed by skin biopsy and successfully treated with statins and steroids. Am J Med Sci 2006; 331: 280-283. PubMed: https://pubmed.ncbi.nlm.nih.gov/16702800/