More Information
Submitted: August 02, 2023 | Approved: August 12, 2023 | Published: August 14, 2023
How to cite this article: Chaovarin C, Tangwonglert T, Supaporn T, Treesit I, Euswas K, et al. Oculars Pain and Intraocular Hypertension in Hemodialysis Patient with Glaucoma: A Case Report and Review of the Literatures. J Clini Nephrol. 2023; 7: 063-066.
DOI: 10.29328/journal.jcn.1001111
Copyright License: © 2023 Chaovarin C, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Resistance hypertension; Intraocular pressure; Ocular dialysis disequilibrium; End stage kidney disease; Hemodialysis
Oculars Pain and Intraocular Hypertension in Hemodialysis Patient with Glaucoma: A Case Report and Review of the Literatures
Chokchai Chaovarin1 , Theerasak Tangwonglert1, Thanom Supaporn1, Isaraporn Treesit2, Krischon Euswas2 and Naowanit Nata1*
, Theerasak Tangwonglert1, Thanom Supaporn1, Isaraporn Treesit2, Krischon Euswas2 and Naowanit Nata1*
1Division of Nephrology, Department of Medicine, Phramongkutklao Hospital, Bangkok, Thailand
2Department of Ophthalmology, Phramongkutklao Hospital, Bangkok, Thailand
*Address for Correspondence: Naowanit Nata, Division of nephrology, Department of Medicine, Phramongkutklao College of Medicine 315 Ratchvidhi Rd. Thung Phayathai, Ratchathewi Bangkok 10400. Thailand, Email: [email protected]
Resistance hypertension in hemodialysis patient usually is common and sometimes difficult to get achieved target blood pressure control. In patient with intradialytic hypertension, eye pain may occur which can be relate to the severity of the hypertension itself. Hemodialysis has relationship to Intraocular Pressure (IOP). Hemodialysis was be Increased Intraoccular Pressure (IOP) and may be the cause of eye pain during hemodialysis due to ocular dialysis disequilibrium. And this receives inadequate attention by nephrologist as a cause of intradialytic hypertension. In this article, we report a patient with resistant hypertension who complain of right eye pain during and after dialysis. After anterior chamber tapping and the aqueous humor was drained. The symptoms and hypertension improved. Undetected significant increase in IOP during hemodialysis may lead to permanent optic nerve damage and should be recognized as a cause of hypertension. An interesting point of this report was the intraocular hypertension get worsed in hemodialysis patients and could be a cause of resistance hypertension. We suggest regular ophthalmologic evaluation in ESKD (End Stage Kidney Disease) patients should be necessary especially in the patient with poorly controlled hypertension, have previous glaucoma, diabetic retinopathy, eye pain, blurred vision, conjunctivitis and headache.
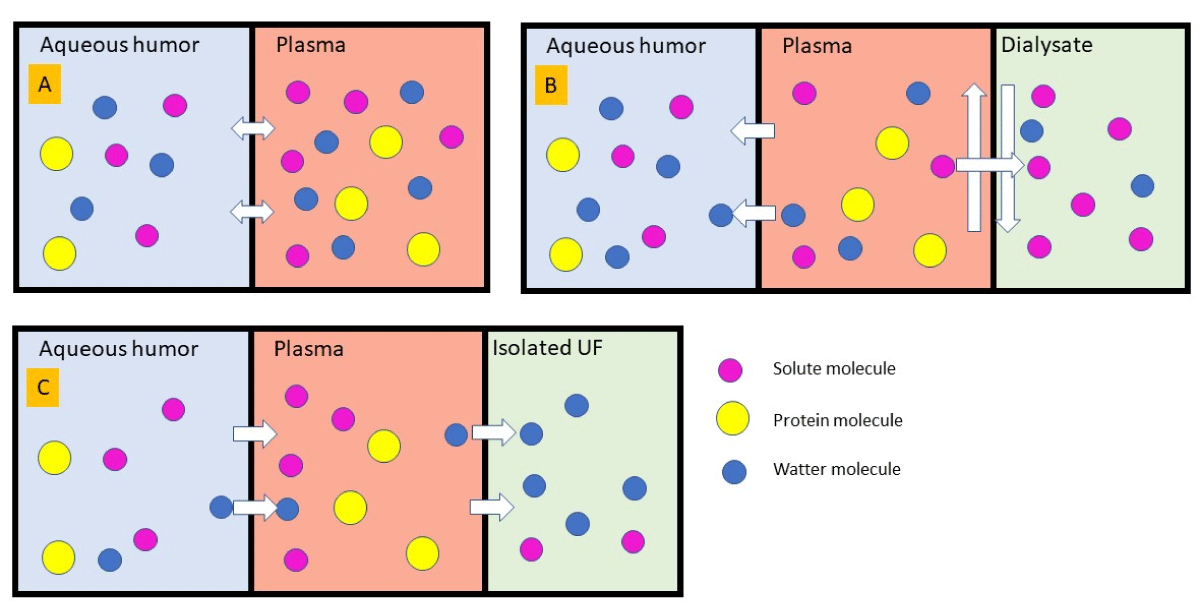
Eye pain during Hemodialysis (HD) is a rare presentation and often goes unfocused in clinical practice. The relationship between Intraocular Pressure (IOP) and hemodialysis was first documented in 1964 by Sitprija, et al. [1]. The reported evidences of IOP during hemodialysis have different variations. According to review of literature, some publications concluded an IOP increase during or after hemodialysis, while other reports showed a decrease in IOP during hemodialysis or no change. Proposed theories for explanation of IOP changes during HD are a rapid decrease in plasma osmolality and relative increase in the concentration of urea in the aqueous humor [2]. The main mechanism is the extracellular fluid shift from the blood compartment to anterior chamber. This osmotic shift during hemodialysis was propose as a new terminology “ocular dialysis disequilibrium” by Cassiopia L, et al. [3] Figure 1. Mechanism of ocular dialysis disequilibrium. The two significant risk factors of increased IOP during hemodialysis were reported in a meta-analysis 2021 (53 studies, N 1903), including acetate dialysate use and preexisting glaucoma or impaired aqueous humor outflow tract [4]. An increase in systolic blood pressure, rapid decrease in serum Na, blood urea nitrogen (BUN) and serum osmolarity have been associated with increased IOP. We reported the resistant severe hypertensive patient, presented with right eye pain during and after dialysis. The interesting point of our case show the unrecognized cause of severe hypertension in regular hemodialysis patient was the progression of glaucoma. Elevation of IOP and reduction of ocular perfusion pressure are the main risk factors for progression of glaucoma. Undetected significant increase in IOP during hemodialysis could lead to permanent optic nerve damage and unknown cause of hypertension.
Figure 1: Mechanism of ocular dialysis disequilibrium during hemodialysis (adaptation from Lippold CL, et al. Hemodial Int. 2019 Jul; 23(3): E72–7). A, In steady state water and solute molecule freely disuse between aqueous humor and plasma via semipermeable membrane. B, during hemodialysis, solute diffuse to dialysate fluid result in decrease of plasma tonicity. Free water osmosis to aqueous humor and cause of increase intraocular pressure. C, in situation of convection mode (isolated ultrafiltration) free water was convicted from aqueous humor to plasma and ultrafiltrate to dialysis fluid.
A 51-year-old male with end stage renal disease due to diabetic nephropathy recieving regular hemodialysis in Sep 2021 has T2DM with severe non proliferative diabetic retinopathy, hypertension and dyslipidemia, dialysis vintage for 10 months. He was prescribed 3 session/week of dialysis via left AVF (arteriovenous fistula), duration 4 hour per session.
He was diagnosed with ghost cell glaucoma at right eye in Mar 2021 due to blurred vision and right eye pain with baseline vision acuity 20/125, 20/100 and Intraocular Pressure (IOP) was measured by icare Tonometer probe (TP01) reaching 14 and 12 mmHg in the right and left eyes, respectively. At the onset of first diagnosis of glaucoma, his IOP increased to 23,18 mmHg. The ophthalmologist prescribed topical therapy (Carbonic anhydrase inhibitor, 1% Prednisolone, alpha 2 adrenergic receptor agonist and Prostanoid selective prostaglandin F receptor agonist. After treatment, the patient was relieved from pain there was a decrease in IOP to 14,12 mmHg. Two months ago he developed recurrent right eye pain at an intradialytic session. He complained of right eye pain (pain score 8/10) and throbbing headache located at right temporal area in the 2nd hour after starting hemodialysis and peak symptoms were established at after dialysis. The patients developed uncontrolled hypertension during the use of Furosemide 1000 mg, Manidipine 20 mg, Losartan 100 mg and Bisoprolol 10 mg per day. The pain symptoms completely recovered at 1 - 2 days after dialysis and were recurrent in the next session of dialysis period. On presentation the IOP was 55 and 22 mmHg (normal< 20 mmHg) in right and left eye. His regular dialysis prescription normally takes 4 hours with blood flow rate 300 ml/min, dialysate flow rate 500 ml/min, temperature 36.5 °C, 2.5 L fluid removal, dialysate Na 138 mmol/L, K 2 mmol/L, Ca 2.5 mEq/L, HCO3- 34 mEq/L. His predialysis blood pressure were 180 - 211/90 - 94 mmHg in clinical setting with no signs of volume overload and dry weight was kept at 70 Kg. In this case we adjusted dry weight by blood volume monitoring. This patient had severe eye pain during dialysis and his IOP increased from 55, 22 mmHg (predialysis) to 60, 26 mmHg (2nd hr) and 70, 26 mmHg (post dialysis) in right and left eye (Table 1).
| Table 1: BP and IOP during hemodialysis. | ||||||
| Day of symptoms | Time (IOP) | IOP (mmHg) | Predialysis BP (mmHg) | Post dialysis BP (mmHg) | Symptoms | |
| Right eye | Left eye | |||||
| Day 1 | T0 | 55 | 22 | 211/94 | 156/78 | |
| T2 | 60 | 26 | Eye pain, headache | |||
| T3 | 70 | 26 | ||||
| Anterior chamber tapping | ||||||
| Day 4 | T0 | 23 | 19 | 186/79 | 131/63 | No symptoms |
| T2 | 25 | 30 | ||||
| Day 7 | T0 | 14 | 18 | 201/85 | 199/90 | No symptoms |
| T2 | 14 | 15 | ||||
| Abbreviation: IOP: Intra Ocular Pressure; T0: 15 minute before hemodialysis; T1: 1 hr after start hemodialysis; T2: 15 minute after complete session of hemodialysis. | ||||||
Lab investigation at the onset of severe eye pain during hemodialysis
CBC: Hb 9.7 HCt 31%, WBC 5600/cumm, N 71%, L 21%, Platelet 134,000/cumm BUN 99 mg/dL, Cr 11 mg/dL, Albumin 4.2 mg/dL, Na 134 mmol/L, K 3.8 mmol/L, Cl 93 mmol/L, HCO3- 23 mmol/L, Ca 9.8 mg/dL, P 4 mg/dL, Mg 2.4 mg/dL, FPG 132 mg/dL, HbA1C 6.2%.
Abbreviation
CBC: Complete Blood Count; HCt: Hematocrit; WBC: White Blood Cell; N: Neutrophil; L: Lymphocyte; BUN: Blood Urea Nitrogen; FPG: Fasting Plasma Glucose
After anterior chamber tapping, the eye pain recovery and his IOP decreased with a dramatic response to normal level in 5 days and pre dialysis blood pressure decreased to 150/70 mmHg in a few weeks.
Intraocular pressure change during HD was investigated by worldwide several study. However, the results were varied from decrease, unchanged and increase IOP. Because there have confounding effects such as IOP measurement, patient position during dialysis, history of glaucoma and aqueous outflow tract facility. According to Vachirasakchai V. study, 41 patients with ESRD on HD ware mesured IOP during dialysis in regular supine position. IOP was found to be increased both during HD (2 hours) and significant increased after HD [5-17].
Resistant hypertension is common problem in ESRD. We appreciate to show the case that had a cause of uncontrolled hypertension from eye pain. Undetected significant increase in IOP during hemodialysis can develop without symptoms and it can aggravate eye pain, ciliary injection, blurred vision or headache. The IOP during hemodialysis according to the studies demonstrated the interindividual variability. Interestingly, previous glaucoma and anatomical defect of aqueous humor outflow tract at iridocorneal angle are the main risk factors for increase in IOP during hemodialysis while, in normal the aqueous humor drainage via the canal of Schlemm to the lymphatic drainage can occur. In this this case the patient had regular dialysis and the pain in the eyes is not caused from dialysis disequilibrium, but from the underlying progressive glaucoma which aggravated the symptoms, severe hypertension, and increase in IOP. The pain recovery and blood pressure were controlled after correcting the specific cause of disease by anterior chamber tapping.
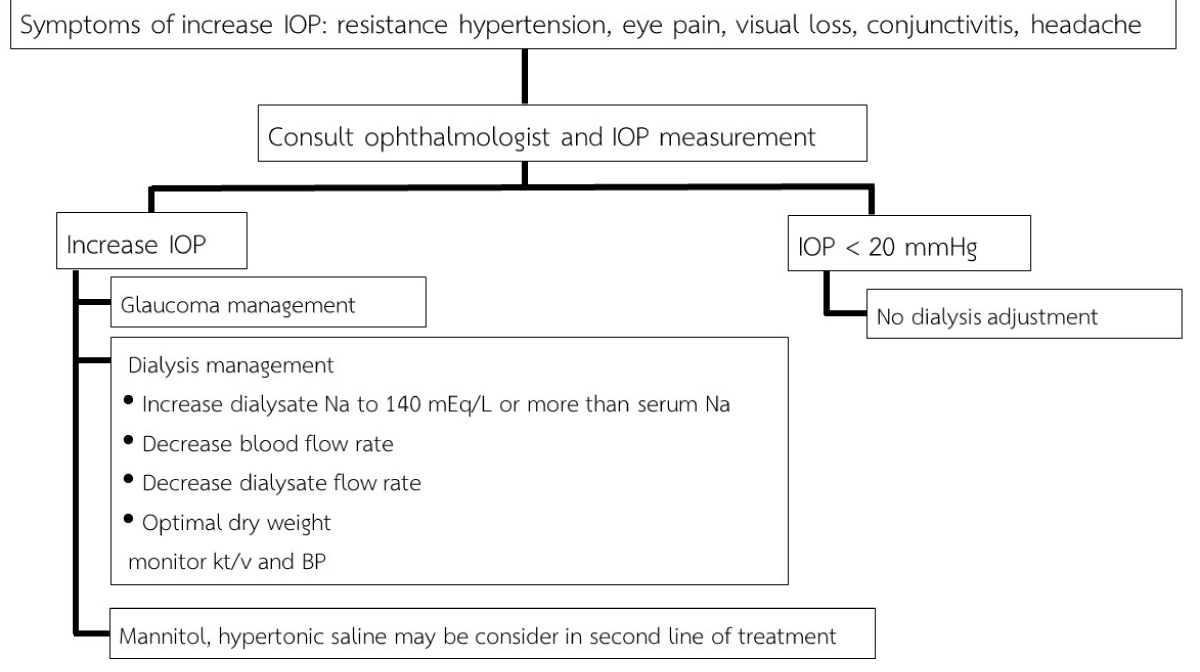
Our management approach of ocular dialysis disequilibrium showed in Figure 2. Dialysis Na should be increase for control tonicity of plasma osmolarity. Decrease blood flow rate and dialysate flow rate for slow urea removal and adjust ultrafiltration rate for control dry weight. Second line treatment was mannitol or hypertonic saline solution intravenous infusion could decrease IOP. In cases failure of medical treatment, shift mode of dialysis to peritoneal dialysis should be consider.
Figure 2: Management approach of ocular dialysis disequilibrium.
An Increase IOP associated with hemodialysis especially in cases have glaucoma, impaired aqueous humor outflow tract. Eye pain during hemodialysis could be a cause of uncontrolled hypertension. An attention to regular ophthalmologic assessment in dialysis patients should be done especially in the patients with risk factors, such as diabetic retinopathy, poorly controlled hypertension, and previous eye diseases.
I would like to thank all the staff and hemodialysis nurse of Nephrology Division at Phramongkutklao Hospital
Disclosure statement
None of the authors have any professional relationships with companies or manufacturers that would benefit from the results of the present study.
Funding
A part of the present study was supported by Biomedical Research and Development Center, Phramongkutklao Hospital.
- Sitprija V, Holmes JH, Ellis PP. Changes in intraocular pressure during hemodialysis. Invest Ophthalmol. 1964 Jun; 3:273-84. PMID: 14169117.
- Levy J, Tovbin D, Lifshitz T, Zlotnik M, Tessler Z. Intraocular pressure during haemodialysis: a review. Eye (Lond). 2005 Dec;19(12):1249-56. doi: 10.1038/sj.eye.6701755. PMID: 15543171.
- Lippold CL, Kalarn SP, Swamy RN, Patel AM. Ocular dialysis disequilibrium-Management of intraocular pressure during hemodialysis of open angle glaucoma: A case report and review of the literature. Hemodial Int. 2019 Jul;23(3):E72-E77. doi: 10.1111/hdi.12718. Epub 2019 Feb 20. PMID: 30785657.
- Chen SH, Lu DW, Ku WC, Chuang LH, Ferng SH, Chen YJ, Lu YH, Chai PY. Changes in Intraocular Pressure During Hemodialysis: A Meta-analysis. J Glaucoma. 2021 Sep 1;30(9):866-873. doi: 10.1097/IJG.0000000000001842. PMID: 33813568.
- Vachirasakchai V. Changes in Intraocular Pressure during and after Hemodialysis. Journal of The Department of Medical Services. 2023; 48(1):67-72.
- Hu J, Bui KM, Patel KH, Kim H, Arruda JA, Wilensky JT, Vajaranant TS. Effect of hemodialysis on intraocular pressure and ocular perfusion pressure. JAMA Ophthalmol. 2013 Dec;131(12):1525-31. doi: 10.1001/jamaophthalmol.2013.5599. PMID: 24232671.
- Tawara A, Kobata H, Fujisawa K, Abe T, Ohnishi Y. Mechanism of intraocular pressure elevation during hemodialysis. Curr Eye Res. 1998 Apr;17(4):339-47. doi: 10.1080/02713689808951214. PMID: 9561825.
- Gafter U, Pinkas M, Hirsch J, Levi J, Savir H. Intraocular pressure in uremic patients on chronic hemodialysis. Nephron. 1985;40(1):74-5. doi: 10.1159/000183431. PMID: 4000337.
- Song WK, Ha SJ, Yeom HY, Seoung GJ, Hong YJ. Recurrent intraocular pressure elevation during hemodialysis in a patient with neovascular glaucoma. Korean J Ophthalmol. 2006 Jun;20(2):109-12. doi: 10.3341/kjo.2006.20.2.109. PMID: 16892647; PMCID: PMC2908824.
- Kilavuzoglu AEB, Yurteri G, Guven N, Marsap S, Celebi ARC, Cosar CB. The effect of hemodialysis on intraocular pressure. Adv Clin Exp Med. 2018 Jan;27(1):105-110. doi: 10.17219/acem/68234. PMID: 29521050.
- Liakopoulos V, Demirtzi P, Mikropoulos DG, Leivaditis K, Dounousi E, Konstas AG. Intraocular pressure changes during hemodialysis. Int Urol Nephrol. 2015 Oct;47(10):1685-90. doi: 10.1007/s11255-015-1043-8. Epub 2015 Jul 4. Erratum in: Int Urol Nephrol. 2015 Oct;47(10):1691. PMID: 26141848.
- Maja AK, Lewis CY, Steffen E, Zegans ME, Graber ML. Increased Intraocular Pressure During Hemodialysis: Ocular Dialysis Disequilibrium. Kidney Med. 2022 Aug 1;4(9):100526. doi: 10.1016/j.xkme.2022.100526. PMID: 36043165; PMCID: PMC9420387.
- Olawoye OO, Ogunleye T, Sarimiye TF, Bello TO. Acute angle closure following hemodialysis in a 34-year-old Nigerian female. Niger J Clin Pract. 2018 Jul;21(7):942-944. doi: 10.4103/njcp.njcp_358_17. PMID: 29984730.
- Saavedra-Fuentes N, Pérez-Grovas H, Navarrete R, Lerma C. Intraocular Pressure Changes During Hemodialysis or Hemodiafiltration in End-Stage Renal Disease Patients. Ther Apher Dial. 2018 Dec;22(6):624-629. doi: 10.1111/1744-9987.12707. Epub 2018 Jul 15. PMID: 30009462.
- Lee WJ, Hong R, Kang MH, Cho H, Han SW, Yi JH, Shin YU, Seong M. Effect of Hemodialysis on Peripapillary Choroidal Thickness Measured by Swept-Source Optical Coherence Tomography. J Glaucoma. 2021 Jun 1;30(6):459-464. doi: 10.1097/IJG.0000000000001762. PMID: 33337722.
- Wang F, Wang L, Yu Z, Chen N, Wang D. Effects of Hemodialysis on Intraocular Pressure and Ocular Biological Parameters in Different Angle Structures. Dis Markers. 2022 Feb 12;2022:9261653. doi: 10.1155/2022/9261653. PMID: 35190757; PMCID: PMC8858050.
- Lerma C, Saavedra-Fuentes N, Ledesma-Gil J, Calderón-Juárez M, Pérez-Grovas H, López-Gil S. Intraocular Pressure Changes during Hemodiafiltration with Two different Concentrations of Sodium in the Dialysate. Biology (Basel). 2021 Dec 23;11(1):12. doi: 10.3390/biology11010012. PMID: 35053010; PMCID: PMC8773306.