More Information
Submitted: January 30, 2023 | Approved: February 07, 2023 | Published: February 08, 2023
How to cite this article: Md Navim Kabir C. Fluctuation of serum creatinine: preoperative and postoperative evaluation of chronic kidney disease patients. J Clini Nephrol. 2023; 7: 012-017.
DOI: 10.29328/journal.jcn.1001102
Copyright License: © 2023 Md Navim Kabir C. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: CKD; Meropenam; NSAID; Co-morbidities; Immobilized
Fluctuation of serum creatinine: preoperative and postoperative evaluation of chronic kidney disease patients
Chowdhury Md Navim Kabir*
Emergency Medical Officer, Islami Bank Central Hospital, Kakrail, Dhaka, Chittagong Medical College, Chattogram, Bangladesh
*Address for Correspondence: Chowdhury Md Navim Kabir, Emergency Medical Officer, Islami Bank Central Hospital, Kakrail, Dhaka, Chittagong Medical College, Chattogram, Bangladesh, Email: [email protected]
Renal impairment is one of the most severe non-communicable diseases around the world. Especially patients with diagnosed/newly diagnosed renal impairment who needed surgery are more focused on preoperative and postoperative preparation. Serum creatinine is the prime biochemical marker for assessing renal function and the level of impairment is widely measured by this marker as well as Glomerular Filtration Rate (GFR).
Objective: Factors responsible for fluctuating serum creatinine during preoperative and postoperative periods and minimizing the process of serum creatinine is the ultimate goal of this study.
Method: 37 patients participated in this cross-sectional study who were previously diagnosed/newly diagnosed. They were admitted to different tertiary-level hospitals for emergency or elective surgery. 15 patients were admitted in the renal function impairment stage and 22 were admitted as normal patients’. Values of creatinine at the pre-admission stage and 2nd/3rd post-admission follow-up were compared.
Results: 0.41 was the average of 22 patients’ creatinine between pre-admission and 2nd/3rd follow-up. The responsible factor like prolonged staying, immobilization, co-morbidities, different preoperative antibiotics and NSAIDs were also inducers for creatinine elevation. After postoperative hemodialysis rapid decrease of creatinine is seen in normal patients but this decrease is very much minor in CKD-diagnosed patients.
Chronic Kidney Disease (CKD) is a common systemic disease worldwide. Due to the lack of a balanced diet along with an unhealthy lifestyle and routine body checkups, many persons become a victim of this disease worldwide, over 800 million people are the victim of this disease. These patients needed persistent monitoring like renal-friendly drug dosage, dietary habits, and lifestyle modification. In the operative procedure, they needed intensive preparation, either emergency or elective. However, cardiological and hematological assessments are routinely done under the supervision of a surgeon and anesthesiologist with direct consultation of a nephrologist. Besides these systemic monitoring, serum creatinine is the prime investigation for assessing kidney function. Satisfactory creatinine levels in serum can be a lifeline for a surgeon and especially for patients point of view who are being immobilized for a long time. For this purpose value of serum creatinine is vital for preoperative and postoperative purposes and fluctuation of this be an obstacle to a patient’s sound preoperative and postoperative preparation.
Biochemical definition of creatinine
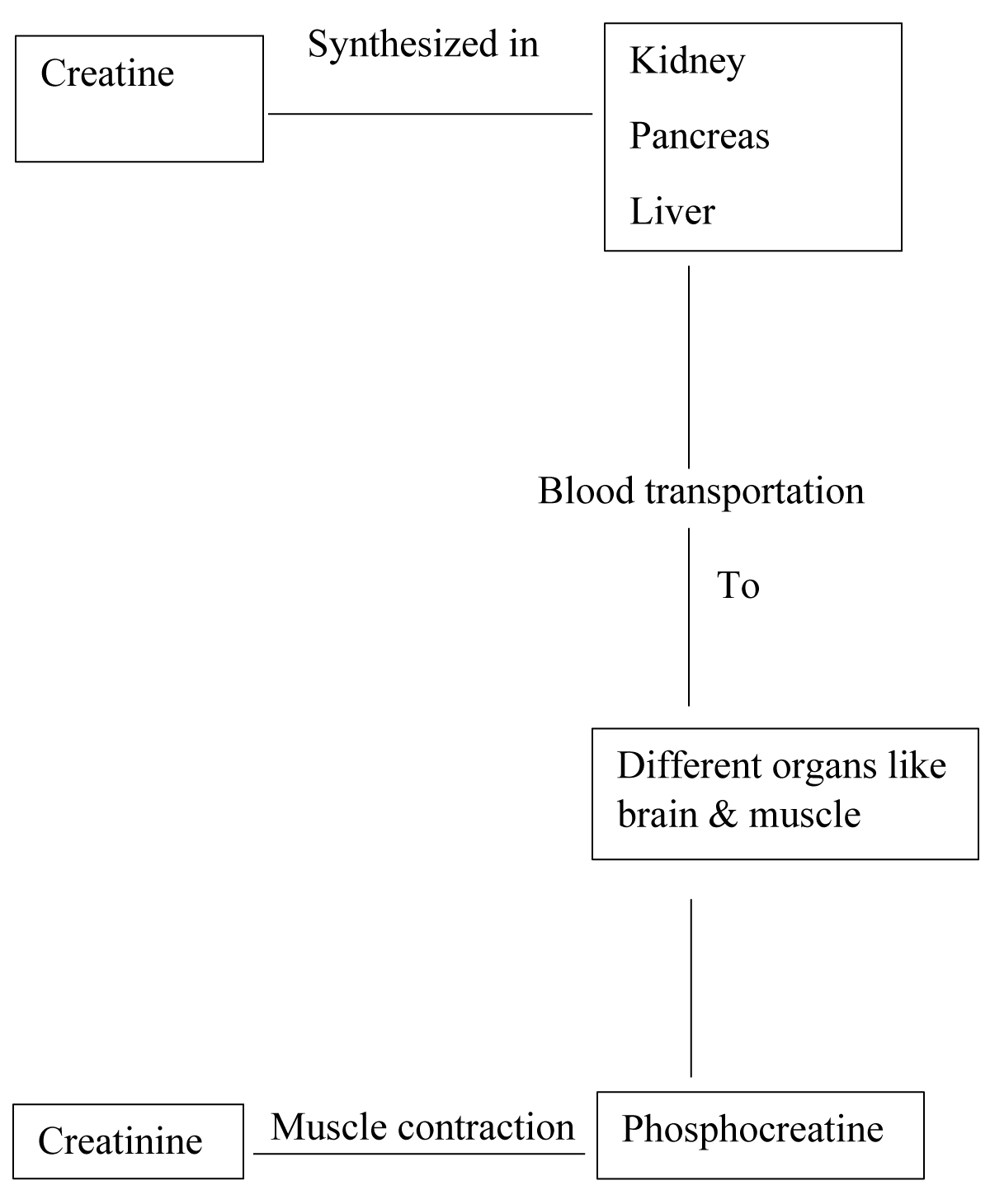
Creatinine is a chemical waste product formed by the breakdown of creatine. It is transported through the bloodstream to the kidneys and washed out. Its production is dependent on muscle mass and the lean muscle mass of a human is directly proportionate to the amount of creatinine in the blood. Creatinine is diet independent, so its concentration depends on the rate at which creatinine is excreted through both kidneys [1,2]
Formation of creatinine (Figure 1).
Figure 1: Diagram of Creatinine Formation [3,4].
Factors of serum creatinine fluctuation
In general thoughts, the elevation of serum creatinine is usually in patients with renal function impairment. But in different cases, the level of creatinine can fluctuate. Normal range of creatinine in healthy males 07 - 1.4 mg/dl and 06 - 1.3 in healthy females. The amount of creatinine can be raised or decreased due to physiological or pathological body conditions. It can be reversible after spontaneous resolution of the underlying condition. Body fluid or electrolytic imbalance can be responsible for this. In acute loose motion, massive fluid loss along with vital minerals. If the dehydration state cannot be corrected, it may be responsible for acute renal impairment with creatinine elevation. In most cases underlying loose motion resolution reverse the kidney function to the normal state. But in some cases, hemodialysis or peritoneal dialysis may be indicated if spontaneous resolution doesn’t occur. As the amount of creatinine is directly related to the muscle bulk, any type of malnutrition may reduce serum creatinine. In the pregnancy period, a reduction of creatinine occurred which physiologically reversed after delivery. Serum creatinine may be fluctuated due to various causes in the preoperative and postoperative periods. It can happen in both old/newly CKD-diagnosed patients or patients of normal renal function. Hydration state, history of high protein diet and long-time immobilization history also play a vital role in creatinine fluctuation in the preoperative and postoperative period. Without systemic emergency and deterioration probability, surgeons and anesthesiologists don’t prefer operative procedures. History of hemodialysis/peritoneal dialysis is also a factor for creatinine fluctuation [5-7].
Analysis of prevalence
A total of 37 participants with an age range of 33 - 67 years participated in this cross-sectional study of those who have a history of creatinine fluctuation in the preoperative/postoperative period during their admission to different tertiary hospitals. 22 of them were male, and 15 of them were female. Out of 22 male participants, 9 were previously CKD diagnosed, and 5 of them took hemodialysis every week. Out of 15 females, 6 were previously CKD diagnosed and 2 of them had a history of hemodialysis. Out of 22 normal male and female participants, 10 patients had previously documented evidence of serum creatinine within the normal range, the sudden rise of creatinine after hospital admission. Out of these 10 patients, 6 were admitted with immobilization history due to road traffic accidents and 4 of them had postoperative complication history. The most important finding was that they had at least one comorbidity (Diabetes Mellitus/hypertension/dyslipidemia) [8-10].
In Table 1, data from 22 patients who had not documented clinical symptoms of renal impairment and normal serum creatinine have been shown. Their serum creatinine during hospital admission and next (2nd/3rd follow up) with hospital duration up to surgery are highlighted. Out of the 22 patients, 4 males and a female need to be hospitalized for 10 days or more than 10 days. Out of the 4 males lowest creatinine value during admission time was 1 mg/dL and the highest was 1.7 mg/dL.1.35 mg/dL is the highest difference between the two creatinine samples of these 4 male patients. The average preoperative hospital admission period is 6 days with a 0.41 average difference of creatinine values in both follow-ups [11-15].
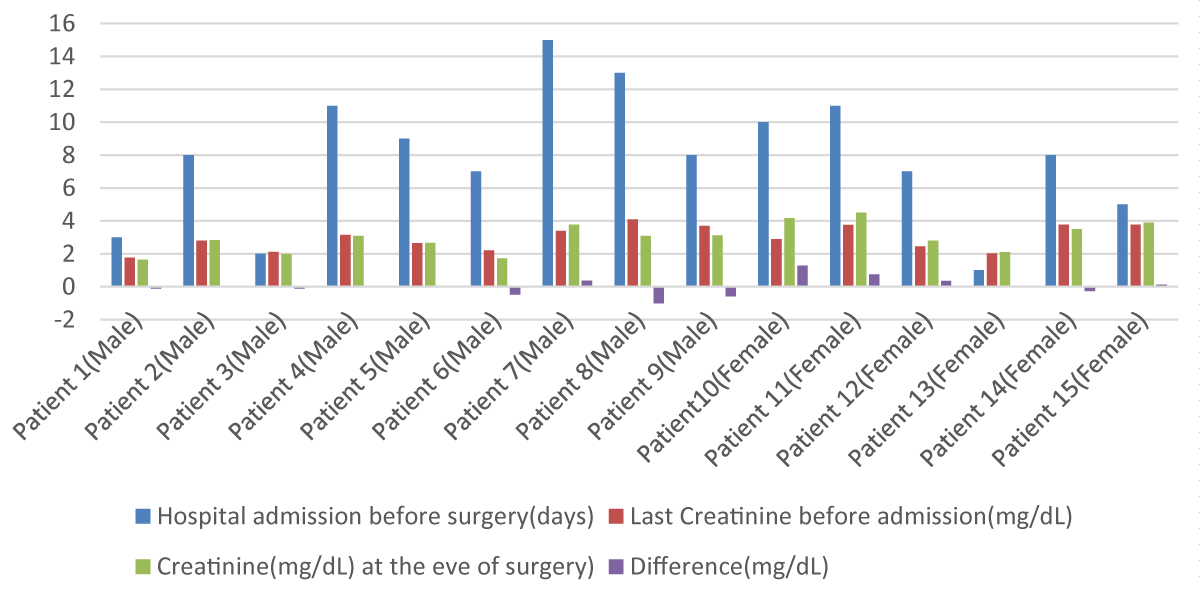
From Table 1 and Figure 2 creatinine fluctuation scenario is highlighted. In Figure 2, 15 patients were previously diagnosed with CKD. Out of 15 patients, 9 were male and 6 were female.5 male patients were documented as hemodialysis takers and 4 weren’t. Out of these 9 patients, 3 of them needed to be hospitalized for more than 10 days and their serum creatinine at the admission was 3.15, 3.4 and 4.01 mg/dL respectively. For preoperative fitness purposes and immobilization avoidance, they need dialysis. The first and third patient’s follow-up creatinine at the eve of surgery were 3.09 and 3.08 mg/dL. These two patients were given hemodialysis and the rest were refused. These 3 patients were highlighted due to their prolonged hospital stay period because of fitness and post-traumatic stability. In comparison, patients who have no history of renal impairment are ahead in fluctuation with patients who were CKD diagnosed. The average creatinine difference of normal patients was 0.41 and 0.02 was the average for impaired patients [16-19].
| Table 1: Patients' Serum Creatinine during Hospital Admission and Next Follow up with Average Summation. | |||||
| Patient and sex | Creatinine at the beginning of admission(mg/dL) X1 |
preoperative hospital duration(days) |
Creatinine at the 2nd/3rd follow-up (mg/dL) X2 |
Difference X2-X1 |
Average ─x= ∑(X2-X1)/N |
| Patient 1 (Male) |
1.25 | 4 | 1.29 | 0.04 | |
| Patient 2 (Male) |
0.99 | 2 | 1.1 | 0.11 | |
| Patient 3 (Male) |
0.73 | 8 | 1.4 | 0.67 | |
| Patient 4 (Male) |
1.4 | 15 | 2.6 | 1.2 | |
| Patien 5 (Male) |
1.11 | 5 | 1.19 | 0.08 | |
| Patient 6 (Male) |
0.75 | 3 | 0.8 | 0.05 | |
| Patient 7 (Male) |
1.18 | 8 | 1.42 | 0.24 | |
| Patient 8 (Male) |
1.7 | 10 | 1.94 | 0.24 | |
| Patient 9 (Male) |
1.1 | 4 | 1.15 | 0.04 | |
| Patient 10 (Male) |
1 | 11 | 2.08 | 1.08 | |
| Patient 11 (Male) |
0.78 | 6 | 1.1 | 0.32 | |
| Patient 12 (Male) |
0.93 | 4 | 0.94 | 0.01 | |
| Patient 13 (Male) |
1.35 | 12 | 2.7 | 1.35 | |
| Patient 14 (Female) |
1.2 | 4 | 1.23 | 0.03 | |
| Patient 15 (Female) |
0.77 | 3 | 0.89 | 0.12 | |
| Patient 16 (Female) |
0.65 | 5 | 0.78 | 0.13 | |
| Patient 17 (Female) |
1.29 | 6 | 1.65 | 0.36 | |
| Patient 18 (Female) |
1.1 | 2 | 1.19 | 0.08 | |
| Patient 19 (Female) |
0.9 | 8 | 1.67 | 0.77 | |
| Patient 20 (Female) |
1.22 | 10 | 2.2 | 0.98 | |
| Patient 21 (Female) |
0.79 | 3 | 0.94 | 0.15 | |
| Patient 22 (Female) |
0.91 | 8 | 1.88 | 0.97 | |
| N = 22 | ∑(X2-X1)=9.02 | 0.41 | |||
Figure 2: Graphical presentation of Creatinine Fluctuation of CKD Diagnosed Patients.
Patients who had high serum creatinine value on the eve of surgery and difference along with prolonged hospital admission staying were given importance especially their postoperative creatinine value as well as postoperative events.
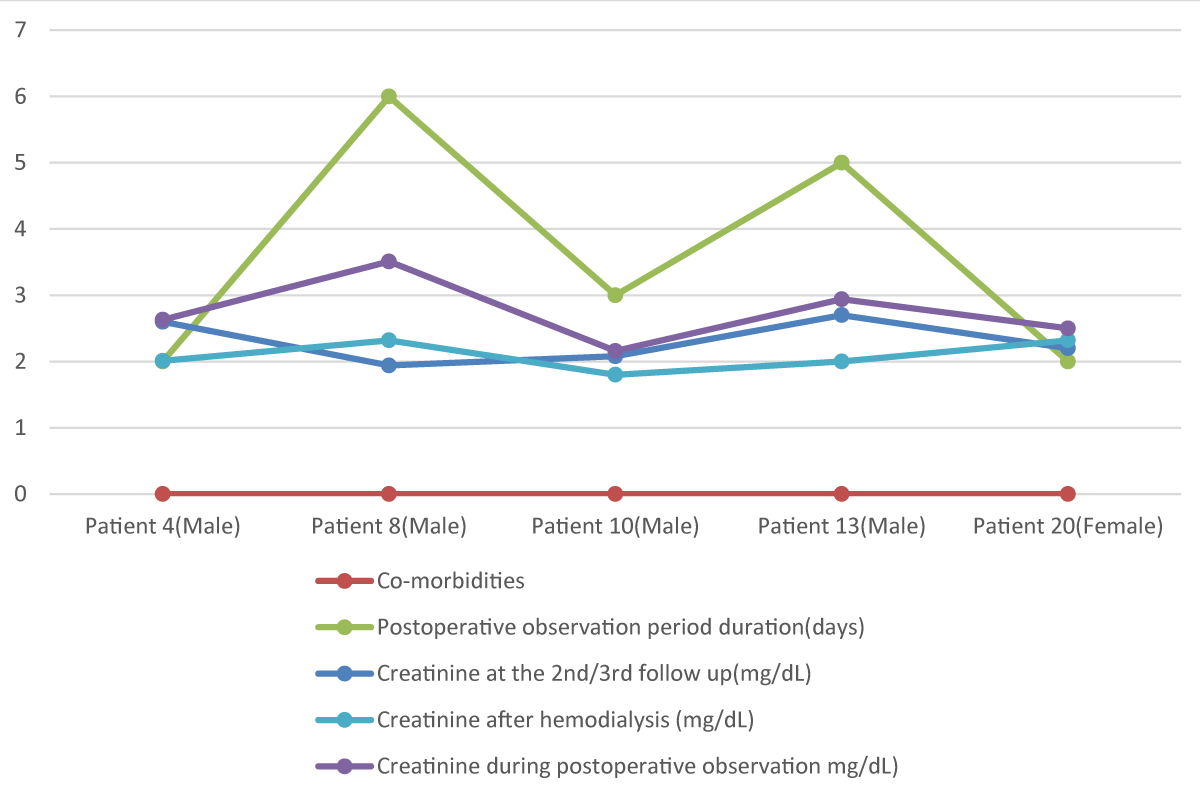
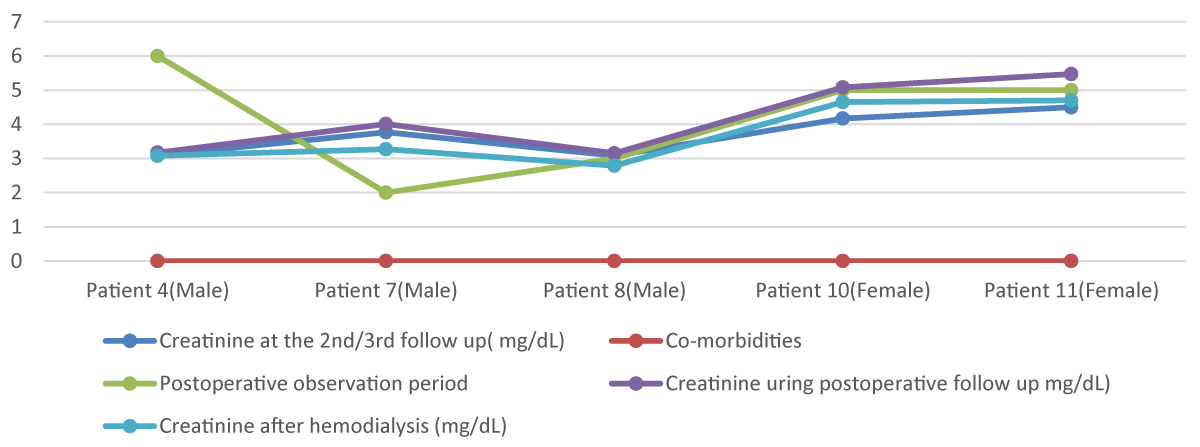
Figure 3 and 4 highlights 37 participants’ serum creatinine fluctuation after surgery. Serum creatinine changing during the postoperative period as well as impacting factors also be highlighted. In Figure 3, 22 patients who had no previous history of renal impairment were admitted for operative purposes and their fluctuation of creatinine before and after dialysis was focused on. Also, the impact of comorbidities on this fluctuation is emphasized. Patients having both DM (Diabetes Mellitus) and HTN (Hypertension) needed to be more postoperative hospitalization than single comorbid patients. Also raising creatinine is mentioned in these multi-comorbid patients. Average fluctuation of creatinine here-0.658 mg/dL. On the other hand, Figure 4 emphasizes the remaining 15 patient’s creatinine who had a history of renal impairment associated with multiple comorbidities. Chiefly DM and HTN had been seen as comorbidities in the patients who needed prolonged postoperative staying (maximum 6 days). Maximum 5.47 mg/dL is the highest postoperative serum creatinine value and 3.15 mg/dL is the lowest. An average differential value between pre-hemodialysis and post-hemodialysis creatinine is -0.618 mg/dL [20-24].
Figure 3: Graphical presentation of Creatinine Fluctuation of Normal Patients in the Postoperative period before and after Hemodialysis.
Figure 4: Graphical presentation of Creatinine Fluctuation of Diagnosed CKD Patients in the Postoperative period before and after Hemodialysis.
Increasing serum creatinine during the postoperative period was triggered by some factors. Especially prolonged preoperative staying, comorbidities and medications in order were responsible for fluctuation.
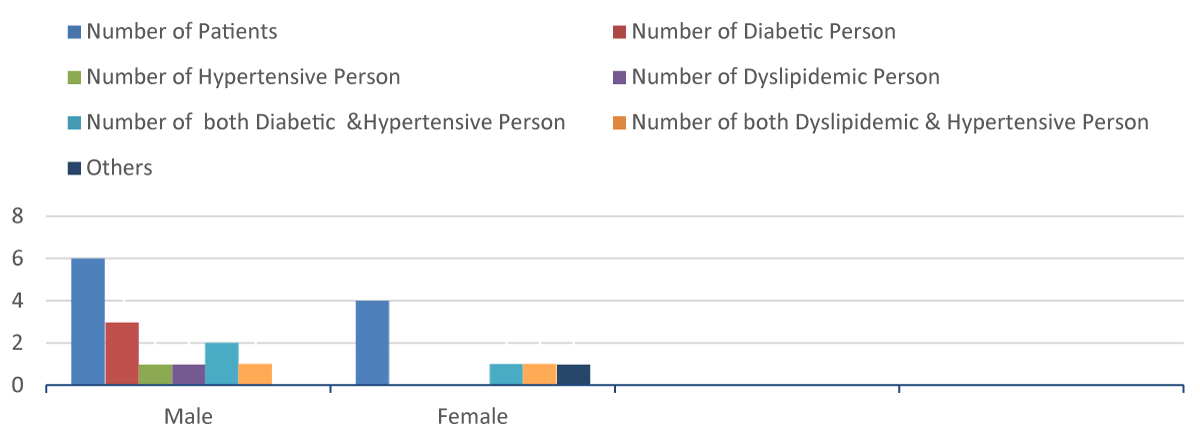
From Figure 5 distribution of comorbidities among patients has been emphasized. Prevalence of diabetes, hypertension and dyslipidemia being showed among the patients. Individually 3 male patient had diabetes and 1 male had hypertension. 3 patients had both diabetes and hypertension where 2 were male and the rest female. These 3 patients had a history of the prolonged post-observation period which may be responsible for rising creatinine. It is also applicable for patients with hypertension and dyslipi-demia due to their 5 days postoperative duration [25-27].
Figure 5: Graphical presentation Showing the Distribution of Different Comorbidities in Normal and CKD Diagnosed Patients.
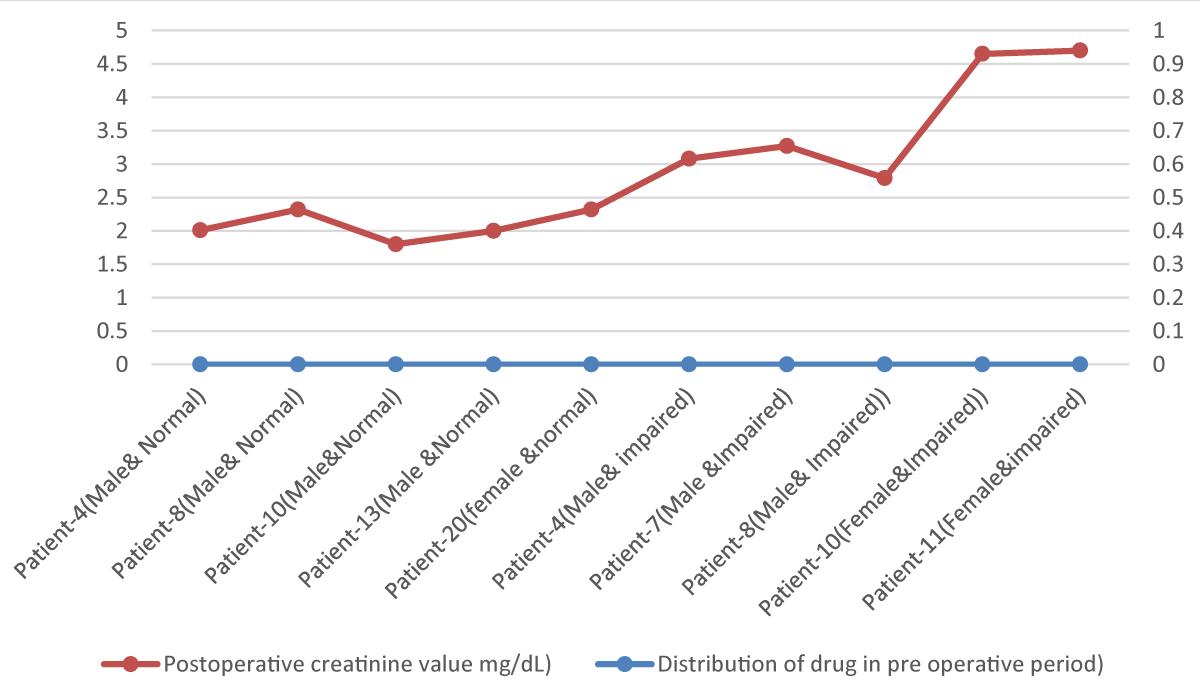
Table 2, Figures 5 and 6 shows the graphical relationship among prescribing drugs history (preoperative and postoperative period) postoperative admission period and the effect upon creatine. Ceftriaxone, meropenem, ketorolac and nabumetone are the drugs that were prescribed before admission and preoperative hospital admission. Patients who weren’t documented as having any kind of renal impairment are typically prescribed ceftriaxone and ketorolac (for relieving pain in road traffic trauma) and serum creatinine was increased with prolonged hospital duration. CKD patients were given meropenem and paracetamol for relieving symptoms. Due to preoperative anesthetic drugs and muscle relaxants, creatinine was increased but after hemodialysis creatinine decreased. In normal patients, fluctuations were more than in the patients who were given dialysis as well as diagnosed with CKD [28].
| Table 2: Patient-Wise Drug Distribution in Pre-Admission and Preoperative Period. | |||||||
| Patient and sex (Normal and Renal impairment) | Pre-admission drug history | Drug name prescribed during the preoperative period | Patient-wise drug distribution during the preoperative period | ||||
| Ceftriaxone | Meropenam | Ketorolac | Meropenam & Ketorolac | Meropenam & Nabumetone |
|||
| Patient-4 (Male & Normal) | Antibiotic | Ceftriaxone | Yes | ||||
| Patient-8 (Male & Normal) | NSAID | Meropenem &Ketorolac | Yes | ||||
| Patient-10 (Male & Normal) | Antibiotic | Ceftriaxone | Yes | ||||
| Patient-13 (Male & Normal) | NSAID | Ceftriaxone | Yes | ||||
| Patient-20 (Female & Normal) | Anti GIT ulcerant | Ceftriaxone | Yes | ||||
| Patient-4 (Male & impaired) | NSAID | Meropenam ¶cetamol | Yes | ||||
| Patient-7(Male & impaired) | NSAID | Meropenam ¶cetamol | Yes | ||||
| Patient-8 (Male & impaired) | Anti GIT ulcerant | Merpenam | Yes | ||||
| Patient-10 (Female & impaired) | Antibiotic | Merpenam | Yes | ||||
| Patient-11 (Female & impaired) | NSAID | Meropenam & Nabumetone | Yes | ||||
Figure 6: Graphical presentation Showing Preoperative Distribution of Different drugs versus postoperative Creatinine Values.
Result with highlighting points: A total of 37 patients participated in this cross-sectional study and 22 patients had no history of kidney disease. On the other hand, the rest of the 15 patients were documented as CKD patients and 7 of them had a history of hemodialysis. These patients were admitted to tertiary-level hospitals for surgery purposes. As baseline investigations, serum creatinine was compared with the pre-admission stage and 2nd/3rd follow-up. The average value of creatinine in 22 normal patients was 0.41. The important finding was the elevation of creatinine after prolonged hospital stays.10 patients needed to stay 10 or more 10 days. Reasons like the preoperative elevation of creatinine, post road traffic accident-induced immobilization triggered that elevation process. Patients’ comorbidity history has also been focused on during the survey. Diabetes, hypertension and dyslipidemia were the main noncommunicable disease responsible for immunosuppression and creatinine elevation. Males were more prone to diabetes and females were dyslipidemia. Those who had more than one disease were very much prone to develop kidney diseases. Besides these pre-admission drug histories as well as after admission different drugs have also been inducers of creatinine elevation. The 10 patients who had prolonged hospital staying history were also habituated to taking antibiotics and NSAIDs on different occasions with/without indications. After admission, Ceftriaxone and ketorolac were also triggering creatinine elevation. Per operative muscle relaxants with anesthetic drugs were also responsible. Postoperative hemodialysis helped mostly for stable kidney function by rapidly reversing the creatinine value. But this fluctuation was very minor it was in the advanced kidney function impairment stage [29-32].
Serum creatinine itself is a gold standard biochemical investigation for assessing renal function. The significance of the kidney in blood pressure management as well as buffer system maintenance, creatinine focus gross renal stability. For different circumstances, elevation and falling of creatinine can occur, which can be assessed by creatinine without delay. For ensuring uneventful per and postoperative period creatinine fluctuation and its inducer events should be properly monitored for rational medical practice.
- Brown JR, Cochran RP, Dacey LJ, Ross CS, Kunzelman KS, Dunton RF, Braxton JH, Charlesworth DC, Clough RA, Helm RE, Leavitt BJ, Mackenzie TA, O'Connor GT; Northern New England Cardiovascular Disease Study Group. Perioperative increases in serum creatinine are predictive of increased 90-day mortality after coronary artery bypass graft surgery. Circulation. 2006 Jul 4;114(1 Suppl):I409-13. doi: 10.1161/CIRCULATIONAHA.105.000596. PMID: 16820609.
- Haase M, Kellum JA, Ronco C. Subclinical AKI--an emerging syndrome with important consequences. Nat Rev Nephrol. 2012 Dec;8(12):735-9. doi: 10.1038/nrneph.2012.197. Epub 2012 Sep 25. PMID: 23007617.
- Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004 Jun;15(6):1597-605. doi: 10.1097/01.asn.0000130340.93930.dd. PMID: 15153571.
- Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999 Mar 16;130(6):461-70. doi: 10.7326/0003-4819-130-6-199903160-00002. PMID: 10075613.
- Tolpin DA, Collard CD, Lee VV, Virani SS, Allison PM, Elayda MA, Pan W. Subclinical changes in serum creatinine and mortality after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2012 Mar;143(3):682-688.e1. doi: 10.1016/j.jtcvs.2011.09.044. Epub 2011 Nov 4. PMID: 22054657.
- Ishani A, Nelson D, Clothier B, Schult T, Nugent S, Greer N, Slinin Y, Ensrud KE. The magnitude of acute serum creatinine increase after cardiac surgery and the risk of chronic kidney disease, progression of kidney disease, and death. Arch Intern Med. 2011 Feb 14;171(3):226-33. doi: 10.1001/archinternmed.2010.514. Erratum in: Arch Intern Med. 2011 Nov 28;171(21):1919. PMID: 21325112.
- Barili F, Pacini D, Rosato F, Roberto M, Battisti A, Grossi C, Alamanni F, Di Bartolomeo R, Parolari A. In-hospital mortality risk assessment in elective and non-elective cardiac surgery: a comparison between EuroSCORE II and age, creatinine, ejection fraction score. Eur J Cardiothorac Surg. 2014 Jul;46(1):44-8. doi: 10.1093/ejcts/ezt581. Epub 2014 Jan 8. PMID: 24401691.
- Stein A, de Souza LV, Belettini CR, Menegazzo WR, Viégas JR, Costa Pereira EM, Eick R, Araújo L, Consolim-Colombo F, Irigoyen MC. Fluid overload and changes in serum creatinine after cardiac surgery: predictors of mortality and longer intensive care stay. A prospective cohort study. Crit Care. 2012 May 31;16(3):R99. doi: 10.1186/cc11368. PMID: 22651844; PMCID: PMC3580649.
- Porter CJ, Juurlink I, Bisset LH, Bavakunji R, Mehta RL, Devonald MA. A real-time electronic alert to improve detection of acute kidney injury in a large teaching hospital. Nephrol Dial Transplant. 2014 Oct;29(10):1888-93. doi: 10.1093/ndt/gfu082. Epub 2014 Apr 16. PMID: 24744280.
- Thomas M, Sitch A, Dowswell G. The initial development and assessment of an automatic alert warning of acute kidney injury. Nephrol Dial Transplant. 2011 Jul;26(7):2161-8. doi: 10.1093/ndt/gfq710. Epub 2010 Dec 8. PMID: 21148028.
- Ji B, Undar A. An evaluation of the benefits of pulsatile versus nonpulsatile perfusion during cardiopulmonary bypass procedures in pediatric and adult cardiac patients. ASAIO J. 2006 Jul-Aug;52(4):357-61. doi: 10.1097/01.mat.0000225266.80021.9b. PMID: 16883112.
- Sickeler R, Phillips-Bute B, Kertai MD, Schroder J, Mathew JP, Swaminathan M, Stafford-Smith M. The risk of acute kidney injury with co-occurrence of anemia and hypotension during cardiopulmonary bypass relative to anemia alone. Ann Thorac Surg. 2014 Mar;97(3):865-71. doi: 10.1016/j.athoracsur.2013.09.060. Epub 2013 Nov 20. PMID: 24266946.
- Ng RR, Chew ST, Liu W, Shen L, Ti LK. Identification of modifiable risk factors for acute kidney injury after coronary artery bypass graft surgery in an Asian population. J Thorac Cardiovasc Surg. 2014 Apr;147(4):1356-61. doi: 10.1016/j.jtcvs.2013.09.040. Epub 2013 Nov 1. PMID: 24183907.
- Aronson S, Phillips-Bute B, Stafford-Smith M, Fontes M, Gaca J, Mathew JP, Newman MF. The association of postcardiac surgery acute kidney injury with intraoperative systolic blood pressure hypotension. Anesthesiol Res Pract. 2013;2013:174091. doi: 10.1155/2013/174091. Epub 2013 Nov 14. PMID: 24324489; PMCID: PMC3845409.
- Stafford-Smith M, Patel UD, Phillips-Bute BG, Shaw AD, Swaminathan M. Acute kidney injury and chronic kidney disease after cardiac surgery. Adv Chronic Kidney Dis. 2008 Jul;15(3):257-77. doi: 10.1053/j.ackd.2008.04.006. PMID: 18565477.
- Eltzschig HK, Collard CD. Vascular ischaemia and reperfusion injury. Br Med Bull. 2004 Oct 19;70:71-86. doi: 10.1093/bmb/ldh025. Erratum in: Br Med Bull. 2005;73-74:139. PMID: 15494470.
- Fox AA, Muehlschlegel JD, Body SC, Shernan SK, Liu KY, Perry TE, Aranki SF, Cook EF, Marcantonio ER, Collard CD. Comparison of the utility of preoperative versus postoperative B-type natriuretic peptide for predicting hospital length of stay and mortality after primary coronary artery bypass grafting. Anesthesiology. 2010 Apr;112(4):842-51. doi: 10.1097/ALN.0b013e3181d23168. PMID: 20216395; PMCID: PMC4988794.
- Fox AA, Nascimben L, Body SC, Collard CD, Mitani AA, Liu KY, Muehlschlegel JD, Shernan SK, Marcantonio ER. Increased perioperative b-type natriuretic peptide associates with heart failure hospitalization or heart failure death after coronary artery bypass graft surgery. Anesthesiology. 2013 Aug;119(2):284-94. doi: 10.1097/ALN.0b013e318299969c. PMID: 23695172; PMCID: PMC3840806.
- Simonini M, Lanzani C, Bignami E, Casamassima N, Frati E, Meroni R, Messaggio E, Alfieri O, Hamlyn J, Body SC, Collard CD, Zangrillo A, Manunta P; CABG Genomics Investigators. A new clinical multivariable model that predicts postoperative acute kidney injury: impact of endogenous ouabain. Nephrol Dial Transplant. 2014 Sep;29(9):1696-701. doi: 10.1093/ndt/gfu200. Epub 2014 Jun 11. PMID: 24920842; PMCID: PMC4200038.
- Collard CD, Gelman S. Pathophysiology, clinical manifestations, and prevention of ischemia-reperfusion injury. Anesthesiology. 2001 Jun;94(6):1133-8. doi: 10.1097/00000542-200106000-00030. PMID: 11465607.
- Sadovnikoff N, Gelman S. Perioperative renal protection. Curr Opin Anaesthesiol. 1999 Jun;12(3):337-41. doi: 10.1097/00001503-199906000-00015. PMID: 17013335.
- Gassanov N, Nia AM, Caglayan E, Er F. Remote ischemic preconditioning and renoprotection: from myth to a novel therapeutic option? J Am Soc Nephrol. 2014 Feb;25(2):216-24. doi: 10.1681/ASN.2013070708. Epub 2013 Dec 5. PMID: 24309187; PMCID: PMC3904574.
- Kaushal GP, Shah SV. Challenges and advances in the treatment of AKI. J Am Soc Nephrol. 2014 May;25(5):877-83. doi: 10.1681/ASN.2013070780. Epub 2014 Jan 30. PMID: 24480828; PMCID: PMC4005310.
- Park SW, Kim M, Kim JY, Ham A, Brown KM, Mori-Akiyama Y, Ouellette AJ, D'Agati VD, Lee HT. Paneth cell-mediated multiorgan dysfunction after acute kidney injury. J Immunol. 2012 Dec 1;189(11):5421-33. doi: 10.4049/jimmunol.1200581. Epub 2012 Oct 29. PMID: 23109723; PMCID: PMC3504173.
- Liotta M, Olsson D, Sartipy U, Holzmann MJ. Minimal changes in postoperative creatinine values and early and late mortality and cardiovascular events after coronary artery bypass grafting. Am J Cardiol. 2014 Jan 1;113(1):70-5. doi: 10.1016/j.amjcard.2013.09.012. Epub 2013 Oct 4. PMID: 24176074.
- Karkouti K, Rao V, Chan CT, Wijeysundera DN, Investigators T. Early rise in postoperative creatinine for identification of acute kidney injury after cardiac surgery. Can J Anaesth. (2017) 64:801-9. doi: 10.1007/s12630-017-0899-8
- Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-84. doi: 10.1159/000339789. Epub 2012 Aug 7. PMID: 22890468.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004 Aug;8(4):R204-12. doi: 10.1186/cc2872. Epub 2004 May 24. PMID: 15312219; PMCID: PMC522841.
- Haase M, Devarajan P, Haase-Fielitz A, Bellomo R, Cruz DN, Wagener G, Krawczeski CD, Koyner JL, Murray P, Zappitelli M, Goldstein SL, Makris K, Ronco C, Martensson J, Martling CR, Venge P, Siew E, Ware LB, Ikizler TA, Mertens PR. The outcome of neutrophil gelatinase-associated lipocalin-positive subclinical acute kidney injury: a multicenter pooled analysis of prospective studies. J Am Coll Cardiol. 2011 Apr 26;57(17):1752-61. doi: 10.1016/j.jacc.2010.11.051. PMID: 21511111; PMCID: PMC4866647.
- Lopez-Delgado JC, Esteve F, Torrado H, Rodríguez-Castro D, Carrio ML, Farrero E, Javierre C, Ventura JL, Manez R. Influence of acute kidney injury on short- and long-term outcomes in patients undergoing cardiac surgery: risk factors and prognostic value of a modified RIFLE classification. Crit Care. 2013 Dec 13;17(6):R293. doi: 10.1186/cc13159. PMID: 24330769; PMCID: PMC4056889.
- Gomez H, Ince C, De Backer D, Pickkers P, Payen D, Hotchkiss J, Kellum JA. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock. 2014 Jan;41(1):3-11. doi: 10.1097/SHK.0000000000000052. PMID: 24346647; PMCID: PMC3918942.
- Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022 Apr;12(1):7-11. doi: 10.1016/j.kisu.2021.11.003. Epub 2022 Mar 18. PMID: 35529086; PMCID: PMC9073222.