More Information
Submitted: March 15, 2022 | Approved: April 05, 2022 | Published: April 06, 2022
How to cite this article: Kahindo CK, Mukuku O, Wembonyama SO, Tsongo ZK. Assessment of knowledge of acute kidney injury among non-nephrology healthcare workers in North-Kivu Province, Democratic Republic of the Congo. J Clini Nephrol. 2022; 6: 030-035.
DOI: 10.29328/journal.jcn.1001087
Copyright License: © 2022 Kahindo CK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Acute renal failure; Knowledge; Practices; Health care workers
Abbreviations: ACE Inhibitors: Angiotensin-Converting Enzyme Inhibitors; AKI: Acute Kidney Injury; ARVs: Antiretrovirals; CKD: Chronic Kidney Disease; DRC: Democratic Republic of the Congo; HCWs: Healthcare Workers; NSAIDs: Non-Steroidal Anti-Inflammatory Drugs
Assessment of knowledge of acute kidney injury among non-nephrology healthcare workers in North-Kivu Province, Democratic Republic of the Congo
Charles Kangitsi Kahindo1,2, Olivier Mukuku3*, Stanis Okitotsho Wembonyama4 and Zacharie Kibendelwa Tsongo5
1Faculty of Medicine, University of Goma, Goma, Democratic Republic of the Congo
2Clinique Internationale Médecine Avancée de au Kivu, Goma, Democratic Republic of the Congo
3Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic Republic of the Congo
4Faculty of Medicine, University of Lubumbashi, Lubumbashi, Democratic Republic of the Congo
5Faculty of Medicine, University of Kisangani, Kisangani, Democratic Republic of the Congo
*Address for Correspondence: Olivier Mukuku, Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic Republic of the Congo, Email: [email protected]
Background: Assessment of knowledge of acute kidney injury (AKI) among healthcare workers (HCWs) is necessary to identify areas of deficiency and key topics to focus on while organizing educational programs to improve AKI care. The objective of this study was to assess AKI knowledge and practice among health care providers in North Kivu province, the eastern Democratic Republic of the Congo.
Material and methods: This was a cross-sectional study conducted in six public hospitals in North Kivu province using a self-administered questionnaire.
Results: A total of 158 HCWs completed the survey, among them 66 (41.78%) were physicians. The mean age of respondents was 36.07 ± 10.16 years and the male gender was 56.33%. Only 12 (7.59%) of the respondents had a good knowledge of the definition and classification of AKI. The respondents’ mean scores were 6.76 out of a total of 18 about risk factors for AKI and 6.29 out of a total of 11 with regard to nephrotoxic drugs. Regarding practices, 28.48% of the respondents assess the risk of AKI in their patients in their daily practices; 31.65% report AKI in the patients’ medical history, and 33.54% call on a nephrologist specialist to get specialized advice.
Conclusion: This study found considerable gaps in knowledge and practice regarding AKI among most of HCWs in North Kivu province.
Acute kidney injury (AKI) is a syndrome of abrupt loss of renal excretory function, often accompanied by rapid failure of renal function [1,2]. This syndrome, due to a sudden drop-in glomerular filtration rate, results in an inability of the kidney to eliminate products of nitrogenous metabolism (urea, creatinine, uric acid, etc.) associated with acid-base loss of control, hydro-electrolytic, hormonal, and even osmotic balances [3,4]. AKI leads to a complex clinical disorder that is associated with high morbidity and mortality despite technological progress in the management of continuous renal replacement therapy leading to unsatisfactory results [5].
Causes of AKI in high-income countries differ from those in resource-limited settings, and clinical outcomes are poorer in the latter [6]. The poorer outcomes are attributed to delayed referral, inadequate diagnostic equipment, and other infrastructural deficiencies, as well as a limited number of clinicians able to provide optimal management [7,8]. Several recent studies have shown that AKI is not only an independent risk factor for in-hospital mortality, but is also associated with progression to chronic kidney disease (CKD) and increased long-term mortality and cardiovascular events [3,9].
Evidence of the increasing incidence of AKI has led to an emphasis on prevention or early management [10]. Early diagnosis of AKI is fundamental to ensure prompt and appropriate management, and to avoid progression to more fatal stages of the disease [2,11].
Most AKI can be prevented or managed by relatively simple measures, such as fluid replenishment, identification, and treatment of the underlying condition (e.g. sepsis and antibiotics), discontinuation of nephrotoxic drugs, and exclusion of obstructive causes [4,9]. Knowledge of these relatively basic measures can correct impaired renal function in a large proportion of AKI cases [8,12]. As Lewington, et al. have previously pointed out [13] in our daily practice, we find that the majority of patients with AKI are initially managed by non-specialists due to the scarcity of nephrologists relative to the prevalence of AKI. Previously, Khan, et al. [14] reported that less than one-third of patients with AKI were seen by nephrologists. Adequate knowledge about AKI is needed among health workers, especially physicians and nurses, to ensure prompt diagnosis and effective management of patients with AKI [15]. A study in Blantyre, Malawi, reported that the majority of health workers were not confident in the management of AKI due to their clinical inexperience and lack of knowledge about AKI management [16]. Improving awareness of AKI in health facilities (facilities) through case-based learning, workshops or periodic visits by a nephrologist will have a positive effect on the knowledge of healthcare workers (HCWs) [1].
Thus, there is a need to assess knowledge of AKI among health care workers in order to identify areas of missing knowledge that should be emphasized in the organization of educational programs to improve the management of AKI. The objective of this study was to assess the knowledge and practice of AKI management among non-nephrology HCWs in various health facilities in North Kivu Province, in the Democratic Republic of the Congo (DRC).
Setting and studying population
This was a cross-sectional study conducted over a twelve-week period from August to October 2021 in public and private hospitals in the North Kivu Province in eastern DRC. A simple random technique was adopted to select the participants, who were physicians and nurses working in the selected health facilities (chosen by reasoned choice in view of their referral nature and the number of the population they serve) and visited in the cities of Goma and Butembo in North Kivu province. Six health facilities, including Virunga General Referral Hospital, Kitatumba General Referral Hospital, Katwa General Referral Hospital, Kyeshero Hospital Center, Saint Vincent de Paul Neuropsychiatric Center, and North Kivu Provincial Hospital, were selected for the study. Each selected health facility was visited by a pair of trained interviewers to collect data according to the ad hoc survey.
We conducted a survey among HCWs using a pre-designed questionnaire that was transferred to the KOBocollect software on tablets in various selected private and public health facilities.
Finally, a total of 10 investigators were recruited. HCWs working in administrative departments were excluded from the survey. The investigators explained the purpose and the procedure of the study and obtained the informed written consent of each respondent before asking them to complete the questionnaire. On a mean, the investigation lasted 10 to 15 minutes. The entire returned questionnaire was examined by the investigators, the missing elements (if any) being modified through additional on-site interviews.
After the explanation, all HCWs (physicians and nurses) who are not working in the nephrology department and who agreed to answer our questionnaire were selected. The total number of HCWs who are not working in the nephrology department in the selected health facilities was 224. All were selected for the study; of these, 40 refused to participate in the study, and 26 were absent during the data collection period. The final sample was 158. The response rate was 79.8%.
Data collection
Knowledge and management practices concerning AKI were assessed using a validated structured closed-ended questionnaire with 16 items in three sections (A, B, and C).
Section A included questions on demographic information (age and gender), number of years of professional experience, and medical title (physician or nurse). Section B consisted of questions assessing knowledge of AKI (AKI’s definition and classification, AKI’s risk factors, and potentially nephrotoxic drugs). Section C consisted of questions related to practice in the management of AKI. The items were reviewed by a nephrologist who made revisions that were relevant to their applicability. These revisions focused on the clarity of the questions and the relevance of the content. The questionnaire was completed by the participants under the supervision of investigators who ensured that the relevant data were correctly reported.
The assessment of knowledge level about AKI was based on the answers (“true”, “false”, or “I don’t know”) regarding topics of risk factors and nephrotoxic drugs. One point was awarded for each correct answer and zero points for a wrong answer. The total score varies by topic as follows:
- Knowledge of risk factors for AKI (18 points)
- Knowledge of nephrotoxic drugs (11 points)
Statistical analysis
The data collected were analyzed using STATA version 16 statistical software to assess the knowledge and practices of health care workers in relation to AKI. Statistical analysis included percentage, mean, and standard deviation. Pearson’s Chi-square test was used to test the association of medical title (physician or nurse) with variables in sections B (knowledge of risk factors for AKI and potentially nephrotoxic drugs) and C (AKI management practices). Statistical significance was reported with a p - value of less than 0.05.
Ethical considerations
Ethical clearance was obtained from the Medical Ethics Committee of the University of Goma (Approval No. UNICOM/CEM/002/20021). Informed consent was obtained from each participant. All copies of the questionnaire were coded (without names), and confidentiality of responses was maintained throughout the study.
A total of 158 HCWs completed the survey, of which 66 (41.78%) were physicians. The mean age of the respondents was 36.07 ± 10.16 years and the male gender was 56.33% (a sex ratio of 1.29). On mean, the respondents had 7.34 years of clinical experience (Table 1).
| Table 1: Demographic and professional characteristics of respondents. | ||
| Variable | Number (n = 158) | Percentage |
| Age (years) | ||
| 20-29 | 51 | 32.28 |
| 30-39 | 54 | 34.18 |
| 40-49 | 35 | 22.15 |
| ≥ 50 | 18 | 11.39 |
| Mean ± SD | 36.07 ± 10.16 | |
| Gender | ||
| Female | 69 | 43.67 |
| Male | 89 | 56.33 |
| Médical title | ||
| Physician | 66 | 41.78 |
| Nurse | 92 | 58.23 |
| Clinical experience (years) | ||
| ≤ 5 | 84 | 53.16 |
| > 5 | 74 | 46.84 |
| Mean ± SD | 7.34 ± 6.78 | |
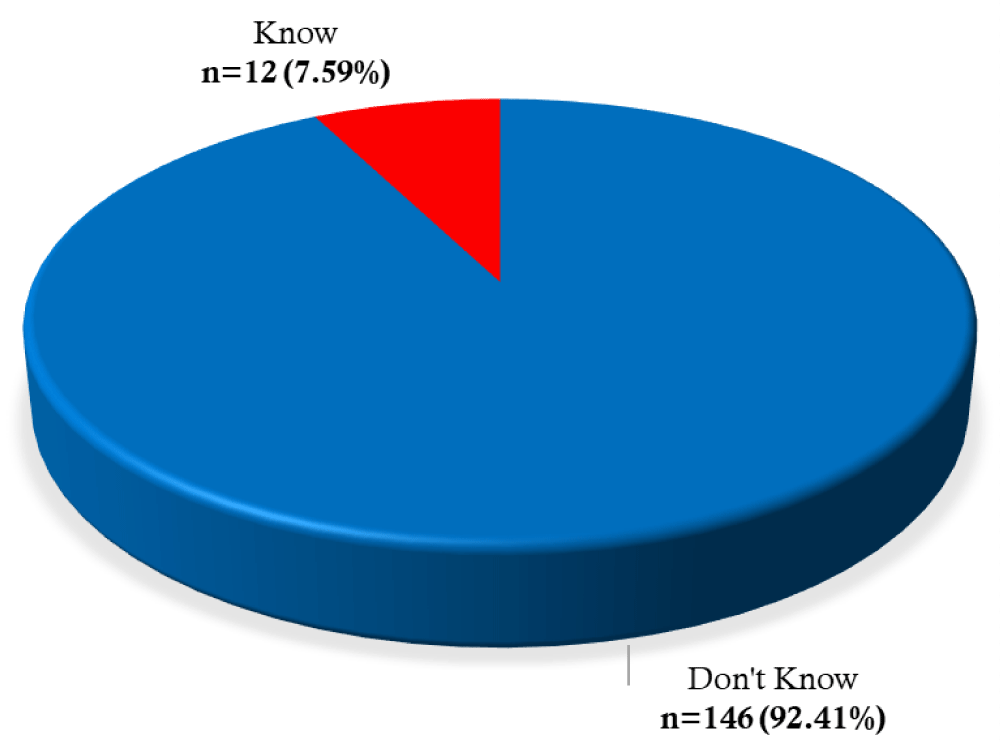
Of all respondents, only 12 (7.59%) were aware of the definition and classification of AKI (Figure 1).
Figure 1: Distribution of respondents according to the knowledge of the definition/classification of AKI.
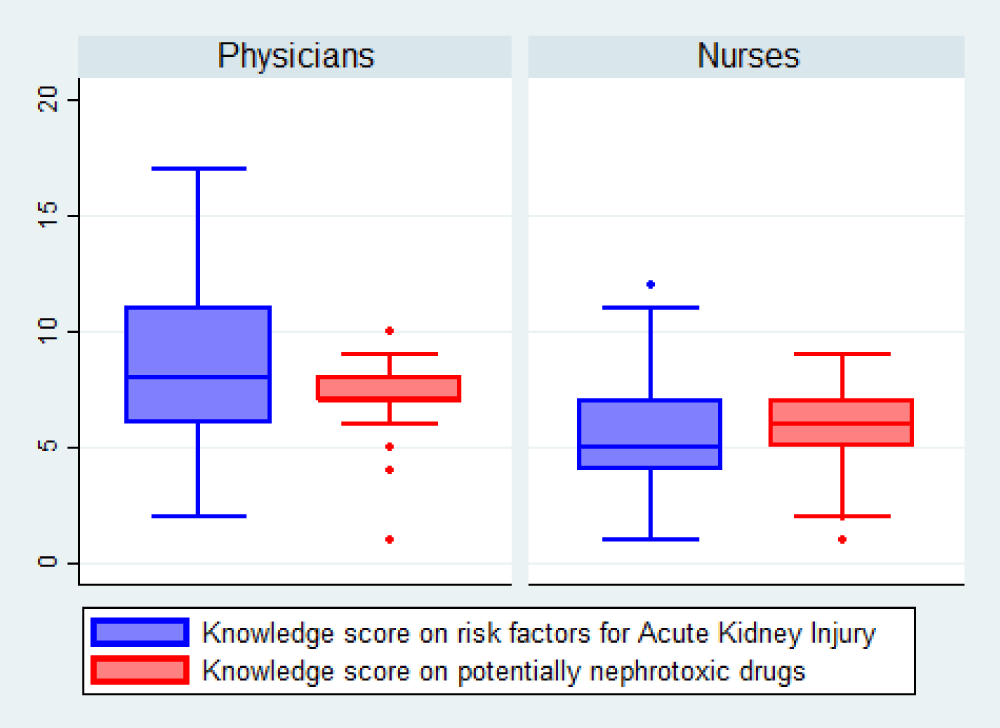
In terms of risk factors knowledge for AKI and potentially nephrotoxic drugs, the mean ratings per topic obtained by the respondents are shown in Figure 2. With regard to risk factors for AKI, the mean score of respondents was 6.76 ± 3.30 out of a total of 18. For the topic of nephrotoxic drugs, the mean score of respondents was 6.29 ± 1.96 out of a total of 11. Comparing the mean scores for these two topics for physicians and nurses, the Student’s t-test shows a highly significant difference (p < 0.0001). The mean scores were 8.80 ± 3.45 and 7.05 ± 1.96 for physicians and 5.30 ± 4.83 and 5.75 ± 1.79 for nurses respectively for risk factors for AKI and potentially nephrotoxic drugs (Figure 2).
Figure 2: Distribution of respondents according to mean knowledge scores..
The percentages of correct answers to questions on knowledge of risk factors for AKI were calculated (Table 2). We noted statistically higher proportions of physicians than nurses in the majority of risk factors (p < 0.05). Overall, we noted that few respondents knew trauma (17.09%), surgery (14.56%), advanced age (22.15%), HIV infection (22.15%), and poisons (24.68%) as risk factors for AKI.
| Table 2: Percentages of respondents with correct answers to knowledge about risk factors for AKI. | ||||
| Risk factor (correct answer) | Medical title | Total (N = 158) | p - value | |
| Physician (n = 66) | Nurse (n = 92) | |||
| Anemia (True) | 25 (37.88%) | 12 (13.04%) | 37 (23.42%) | < 0.001 |
| Trauma (True) | 13 (19.70%) | 14 (15.22%) | 27 (17.09%) | 0.600 |
| Alcohol (False) | 55 (83.33%) | 62 (67.39%) | 117 (74.05%) | 0.038 |
| Bronchial asthma (False) | 66 (100.0%) | 76 (82.61%) | 142 (89.87%) | < 0.001 |
| History of AKI (True) | 22 (33.33%) | 16 (17.39%) | 38 (24.05%) | 0.033 |
| Burn (True) | 25 (37.88%) | 15 (16.30%) | 40 (25.32%) | 0.003 |
| Surgery (True) | 15 (22.73%) | 8 (8.70%) | 23 (14.56%) | 0.025 |
| Dehydration (True) | 37 (56.06%) | 20 (21.74%) | 57 (36.08%) | < 0.001 |
| Diabetes mellitus (True) | 38 (57.58%) | 29 (31.52%) | 67 (42.41%) | 0.001 |
| Gastroenteritis (True) | 31 (46.97%) | 15 (16.30%) | 46 (29.11%) | < 0.001 |
| Hypertension (True) | 42 (63.64%) | 31 (33.70%) | 73 (46.20%) | < 0.001 |
| Sepsis (True) | 39 (59.09%) | 22 (23.91%) | 61 (38.61%) | < 0.001 |
| Chronic kidney disease (True) | 22 (33.33%) | 23 (25.00%) | 45 (28.48%) | 0.334 |
| Poisons (True) | 20 (30.30%) | 19 (20.65%) | 39 (24.68%) | 0.229 |
| Tobacco (False) | 59 (89.39%) | 76 (82.61%) | 135 (85.44%) | 0.335 |
| Indigenous products (True) | 36 (54.55%) | 19 (20.65%) | 55 (34.81%) | < 0.001 |
| Advanced age (True) | 12 (18.18%) | 23 (25.00%) | 35 (22.15%) | 0.410 |
| HIV infection (True) | 16 (24.24%) | 19 (20.65%) | 35 (22.15%) | 0.732 |
The percentages of correct answers to the questions on knowledge of risk factors for AKI were calculated (Table 3).
| Table 3: Percentages of respondents with correct answers to knowledge about nephrotoxic drugs. | ||||
| Nephrotoxic drugs (correct answer) | Medical title | Total (N = 158) | p - value | |
| Physician (n = 66) | Nurse (n = 92) | |||
| NSAIDs (True) | 31 (46.97%) | 25 (27.17%) | 56 (35.44%) | 0.016 |
| Fluconazole (False) | 51 (77.27%) | 83 (90.22%) | 134 (84.81%) | 0.044 |
| ARVs (True) | 18 (27.27%) | 24 (26.09%) | 42 (26.58%) | 1.000 |
| Bactrim (False) | 56 (84.85%) | 62 (67.39%) | 118 (74.68%) | 0.021 |
| Ceftriaxone (False) | 61 (92.42%) | 69 (75.00%) | 130 (82.28%) | 0.009 |
| Ciprofloxacin (False) | 51 (77.27%) | 63 (68.48%) | 114 (72.15%) | 0.300 |
| Gentamycin (True) | 56 (84.85%) | 29 (31.52%) | 85 (53.80%) | < 0.001 |
| ACE inhibitors (False) | 47 (71.21%) | 74 (80.43%) | 121 (76.58%) | 0.246 |
| Chlorpromazine (False) | 55 (83.33%) | 73 (79.35%) | 128 (81.01%) | 0.671 |
| Furosemide (True) | 42 (63.64%) | 31 (33.70%) | 73 (46.20%) | < 0.001 |
| Methotrexate (True) | 21 (31.82%) | 13 (14.13%) | 34 (21.52%) | 0.013 |
| ARVs: Antiretrovirals; NSAIDs: Non-Steroidal Anti-inflammatory Drugs; ACE Inhibitors: Angiotensin-Converting Enzyme Inhibitors. | ||||
We noted statistically higher proportions of physicians than nurses in the majority of drugs (p < 0.05). Overall, we noted that few respondents knew methotrexate (21.52%), antiretrovirals (ARVs) (26.58%), and Non-steroidal anti-inflammatory drugs (NSAIDs) (35.44%), and furosemide (46.20%) as potentially nephrotoxic drugs.
As for practices in the management of AKI, Table 4 shows that 28.39% of the respondents had always/often seen patients with AKI in their practices in the year prior to the survey; 28.48% of the respondents had reported doing a risk assessment of AKI in their patients in their daily practices; 31.65% reported AKI in the medical history of patients who suffered from AKI in the past. One-third (33.54%) of the respondents reported that they seek advice or review risk factors for AKI from a nephrologist specialist for patients who are about to undergo a high-risk procedure or take highly nephrotoxic drugs.
| Table 4: Respondents’ answers to questions on AKI management practices. | ||||
| Practices | Medical title | Total (N = 158) | p - value | |
| Physician (n = 66) | Nurse (n = 92) | |||
| In the past year, have you been confronted with patients suffering from AKI in your practice | 0,001 | |||
| Always | 2 (3.03%) | 69 (16.85%) | 17 (10.97%) | |
| Often | 14 (21.21%) | 13 (14.61%) | 27 (17.42%) | |
| Sometimes | 23 (34.85%) | 13 (14.61%) | 36 (23.23%) | |
| Rarely | 27 (40.91%) | 48 (53.93%) | 75 (48.39%) | |
| In your daily practice, do you assess the risk of AKI in your patients? | 0.006 | |||
| No | 39 (59.09%) | 74 (80.43%) | 113 (71.52%) | |
| Yes | 27 (40.91%) | 18 (19.57%) | 45 (28.48%) | |
| Do you report AKI in the medical history of patients who have suffered from AKI in the past? | < 0.001 | |||
| No | 33 (50.00%) | 75 (81.52%) | 108 (68.35%) | |
| Yes | 33 (50.00%) | 17 (18.48%) | 50 (31.65%) | |
| Do you call a specialist nephrologist for advice or to review the risk factors for AKI for patients who are going to have a high-risk procedure or are taking highly nephrotoxic drugs | 0.011 | |||
| No | 36 (54.55%) | 69 (75.00%) | 105 (66.46%) | |
| Yes | 30 (45.45%) | 23 (25.00%) | 53 (33.54%) | |
The International Society of Nephrology launched the “0 by 25” campaign, which aims to have no patient death from preventable or untreated AKI in low-resource settings by 2025 through screening, diagnosis, and management of patients with AKI. Therefore, it is important to think about the best way to achieve this goal by focusing on particular challenges of resource-limited countries.
This study is a useful tool so that it may provide a lead to how to implement “0 by 25” by first identifying deficits among health providers and thereby enabling the implementation of appropriate changes to improve mortality rates related to AKI.
The present study shows that there are significant gaps in knowledge of AKI among health care providers. Only 12 (7.59%) of the respondents had a good knowledge of the definition and classification of AKI. The mean rating of respondents regarding risk factors for AKI was 6.76 out of a total of 18. As for the knowledge of nephrotoxic drugs, the respondents had a mean score of 6.29 out of a total of 11.
The present study also shows that there are very significant differences between physicians and nurses. This could be explained by different academic training programs in the two groups (physicians and nurses), which explains the insufficient knowledge and the minimal importance given to AKI in nursing schools. This is compounded by the absence of teaching materials on AKI management in the intensive care unit in almost all public hospitals in North Kivu province. Yet nurses play a key role in the early detection and identification of patients with risk factors for AKI. The nurse is also the focal point for monitoring and detecting any abnormalities in patients’ laboratory tests, such as serum creatinine, hemoglobin, or diuresis; these parameters are representative of actual renal function. Abnormal results are immediately reported to the physician so that prompt and appropriate action can be taken. As the results of the present study show, Abdou, et al. [17] also found that the level of knowledge was generally low in the nursing population. A survey of junior physicians in the United Kingdom showed that 30% of the respondents could not name more than two risk factors for AKI and 37% could not name the correct attitudes for referral to a nephrologist [22]. The study by Ali, et al. [1] reported that 23.7% of the respondents did not know whether major surgery was a risk factor for AKI.
Overall, the present study revealed that few respondents were aware of trauma (17.09%), surgery (14.56%), advanced age (22.15%), HIV infection (22.15%), and poisons (24.68%) as risk factors for AKI. This indicates that a significant proportion (over 70%) of the respondents are unable to suspect AKI in these circumstances. Yet trauma induces AKI either through the role of hemolysis or anatomical destruction [18] and surgical stress induces a set of hormonal and hemodynamic modifications linked to anesthesia and mechanical ventilation, thus leading to a deregulation of the renal system, evolving towards AKI [19]. Elderly subjects have reduced functional renal reserve, impaired renal self-regulation, reduced fluid homeostasis, and increased risk of drug nephrotoxicity, making them highly susceptible to AKI [20]. AKI is more common in HIV-infected patients than in HIV-negative patients. It is favored by the viral infection itself, dehydration, undernutrition, opportunistic infections, the role of certain drugs (notably NSAIDs and ARVs), and the immune restoration syndrome [21]. All this information is supposed to be given to respondents during their academic training. This highlights the importance of organizing adequate training sessions on AKI among health care providers, especially physicians and nurses, to ensure rapid and correct diagnosis and effective management of AKI patients.
Overall, we noted that few respondents were aware that methotrexate (21.52%), ARVs (26.58%), NSAIDs (35.44%), and furosemide (46.20%) are known to be nephrotoxic drugs. In contrast, Ali, et al. [1] found that NSAIDs and methotrexate were cited by 76% and 68.6% of health care providers respectively as drugs that cause AKI. Adejumo, et al. [15] found that only 29.6% of respondents recognized furosemide as a risk factor for AKI. Most of these drugs are commonly administered to hospitalized patients and insufficient knowledge about these drugs may prevent physicians from reducing their doses or withdrawing them in people at AKI risk. This may worsen pre-existing AKI or cause iatrogenic AKI. The latter is also associated with a significant burden in terms of healthcare costs, hospital stay, morbidity, and mortality.
Our results show that 28.48% of the respondents assess the risk of AKI in their patients in their daily practice; 31.65% report AKI in the patients’ medical history, and 33.54% seek specialist advice from a nephrologist. These figures are lower than those found by Ali, et al. [1] who reported 72% of respondents assessed the AKI risk in their patients, 57% documented AKI in their medical history and 80.8% called a nephrologist before a high-risk procedure or administration of a nephrotoxic drug. This difference could be explained by the fact that our study population was made up of physicians and nurses unlike the study by Ali, et al. [1] who enrolled only physicians.
To improve the diagnosis of AKI, it is necessary to promote a better understanding of the epidemiological association of AKI with widespread diseases, including endemic diseases, and also to promote education about AKI at all levels and among all members of the health care system. This study highlights the need and importance of better understanding barriers and challenges to implementing an effective AKI management program in resource-poor countries. It is important that each country understands its own barriers in order to implement effective AKI prevention protocols and thus improve the quality of patient’s life.
Data availability: The datasheet used to support the findings of this study are available from the corresponding author upon request.
- Ali SM, Badi S, Yousef BA. Physicians’ knowledge and practice with regard to acute kidney injury at Omdurman Military Hospital: A cross‑sectional survey. Int J Health Allied Sci. 2020; 9: 39-39.
- Nimkar A, Naaraayan A, Hasan A, Pant S, Durdevic M, et al. Incidence and risk factors for acute kidney injury and its effect on mortality in patients hospitalized from Covid-19. Mayo Clin Proc Innov Qual Outcomes. 2020; 4: 687-695. PubMed: https://pubmed.ncbi.nlm.nih.gov/32838205/
- Thongprayoon C, Hansrivijit P, Kovvuru K, Kanduri SR, Torres-Ortiz A, et al. Diagnostics, risk factors, treatment and outcomes of acute kidney injury in a new paradigm. J Clin Med. 2020; 9: 1104. PubMed: https://pubmed.ncbi.nlm.nih.gov/32294894/
- Oates T, Moochhala S. Recognition and management of acute kidney injury. Prescriber. 2017; 28: 17-21.
- Olowu WA, Niang A, Osafo C, Ashuntantang G, Arogundade FA, et al. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2016; 4: e242-e250. PubMed: https://pubmed.ncbi.nlm.nih.gov/27013312/
- Cerdá J, Mohan S, Garcia-Garcia G, Jha V, Samavedam S, et al. Acute kidney injury recognition in low-and middle-income countries. Kidney Int Rep. 2017; 2: 530-543. PubMed: https://pubmed.ncbi.nlm.nih.gov/29034358/
- Kher V, Srisawat N, Noiri E, Gharbi MB, Shetty MS, et al. Prevention and therapy of acute kidney injury in the developing world. Kidney Int Rep. 2017; 2: 544-558. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5720672/
- Liu KD, Forni L, Heung M, Wu VC, Kellum JA, et al. Quality of care for acute kidney disease: current knowledge gaps and future directions. Kidney Int Rep. 2020; 5: 1634-1642. PubMed: https://pubmed.ncbi.nlm.nih.gov/33102955/
- James MT, Hobson CE, Darmon M, Mohan S, Hudson D, et al. Applications for detection of acute kidney injury using electronic medical records and clinical information systems: workgroup statements from the 15th ADQI Consensus Conference. Can J Kidney Health Dis. 2016; 3: 9. PubMed: https://pubmed.ncbi.nlm.nih.gov/26925245/
- Joslin J, Wilson H, Zubli D, Gauge N, Kinirons M, et al. Recognition and management of acute kidney injury in hospitalised patients can be partially improved with the use of a care bundle. Clin Med. 2015; 15: 431. PubMed: https://pubmed.ncbi.nlm.nih.gov/26430180/
- Nascimento RAMD, Assunção MSC, Silva JM, Amendola CP, Carvalho TMD, et al. Nurses’ knowledge to identify early acute kidney injury. Revista da Escola de Enfermagem da USP. 2016; 50: 0399-0404. PubMed: https://pubmed.ncbi.nlm.nih.gov/27556709/
- Igiraneza G, Dusabejambo V, Finklestein FO, Rastegar A. Challenges in the recognition and management of acute kidney injury by hospitals in resource-limited settings. Kidney Int Rep. 2020; 5: 991-999. PubMed: https://pubmed.ncbi.nlm.nih.gov/32647756/
- Lewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney int Rep. 2013; 84: 457-467. PubMed: https://pubmed.ncbi.nlm.nih.gov/23636171/
- Khan IH, Catto GRD, Edward N, Macleod AM. Acute renal failure: factors influencing nephrology referral and outcome. QJM: Int J Med. 1997; 90: 781-785. PubMed: https://pubmed.ncbi.nlm.nih.gov/9536343/
- Adejumo O, Akinbodewa A, Alli O, Olufemi P, Olatunji A. Assessment of knowledge of acute kidney injury among non-nephrology doctors in two government hospitals in Ondo City, Southwest, Nigeria. Ethiop J Health Sci. 2017; 27: 147-154. PubMed: https://pubmed.ncbi.nlm.nih.gov/28579710/
- Evans R, Rudd P, Hemmila U, Dobbie H, Dreyer G. Deficiencies in education and experience in the management of acute kidney injury among Malawian healthcare workers. Malawi Med J. 2015; 27: 101-103. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688871/
- Abdou FA, Abdou SM. Assessment of Nurses knowledge in the early detection and Management of acute kidney injury in Assuit and Mansoura Main University hospital. J Health Sci Nurs. 2019; 4: 47-60.
- Batouche DD, Benatta NF, Sadaoui L, Okbani R, Mentouri Z. L’insuffisance rénale aiguë post-traumatique chez l’enfant et facteurs prédictifs de sa survenue. Néphrologie Thérapeutique. 2016; 12: 320-321.
- Blayau C. Insuffisance rénale aiguë postopératoire. Le Praticien en Anesthésie Réanimation. 2011; 15: 352-358.
- Davidman M, Olson P, Kohen J, Leither T, Kjellstrand C. Iatrogenic Renal Disease. Arch Int Med.1991; 151: 1809-1812. PubMed: https://pubmed.ncbi.nlm.nih.gov/1888247/
- Izzedine H. Pathologies rénales au cours de l’infection par le VIH. La lettre de l’infectiologue. 2009; 24: 146-156.
- Muniraju TM, Lillicrap MH, Horrocks JL, Fisher JM, Clark RMW, et al. Diagnosis and management of acute kidney injury: deficiencies in the knowledge base of non-specialist, trainee medical staff. Clin Med. 2012; 12: 216-221. PubMed: https://pubmed.ncbi.nlm.nih.gov/22783771/